A health history form, or medical history form, is the cornerstone of patient care. It provides healthcare providers with a crucial, comprehensive background, enabling them to make accurate diagnoses, develop appropriate treatment plans, and ensure patient safety.
Understanding the components and best practices for completing this document is essential for both patients and clinicians.
1. What is a Health History Form?
A health history form is a standardized, structured document used to record a patient’s past and present health status. It is typically completed by the patient before their first visit and is used by the physician, nurse, or other medical professional to guide the initial consultation and subsequent care.
The form acts as a foundational medical record, creating a narrative that links a patient's current symptoms to their lifestyle, past illnesses, family predispositions, and current medications. It is a critical component of the subjective data collected during a SOAP (Subjective, Objective, Assessment, Plan) note process.
2. Why is the Medical History Form Important?
The Medical History Form is a vital tool for comprehensive healthcare for several key reasons:
- Diagnostic Clues: Symptoms that appear unrelated in isolation often reveal patterns when viewed against the backdrop of family history or past illnesses. For example, a new joint ache gains significance if the patient has a family history of autoimmune disease.
- Risk Assessment: It identifies risks related to allergies, drug interactions, or conditions that might contraindicate specific treatments (e.g., using certain contrast dyes in a patient with kidney disease).
- Preventive Care: Information on lifestyle (smoking, diet, exercise) and family history of chronic diseases (cancer, diabetes) allows providers to recommend targeted screenings and lifestyle modifications.
- Legal Documentation: The completed and signed form is a legal document that confirms the patient provided relevant information to the provider, forming part of the official medical record.
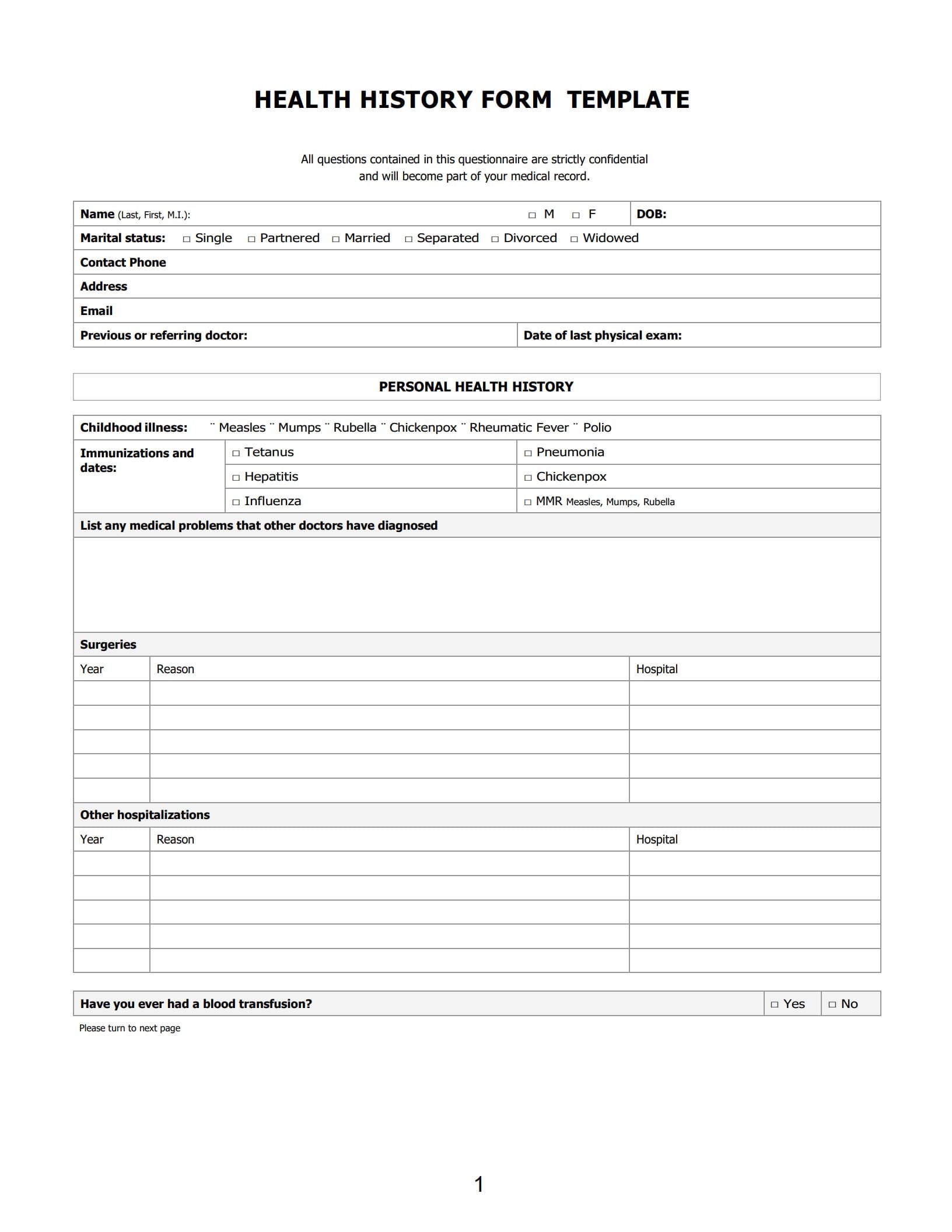
3. What are the Components of a Health History Form?
A comprehensive health history form is typically divided into several distinct, mandated sections to ensure all areas of a patient's health are covered.
The key components of a medical history form
- Biographical Data: Patient’s name, date of birth (DOB), gender, contact information, emergency contact, and insurance details.
- Chief Complaint (CC): A brief, focused statement describing the primary reason for the visit, ideally in the patient's own words (e.g., "Sharp pain in lower back since Tuesday").
- History of Present Illness (HPI): Detailed exploration of the Chief Complaint using the COLDSPA mnemonic (Character, Onset, Location, Duration, Severity, Pattern, Associated factors).
- Past Medical History (PMH): A record of childhood and adult illnesses, surgeries, hospitalizations, serious injuries, and immunizations.
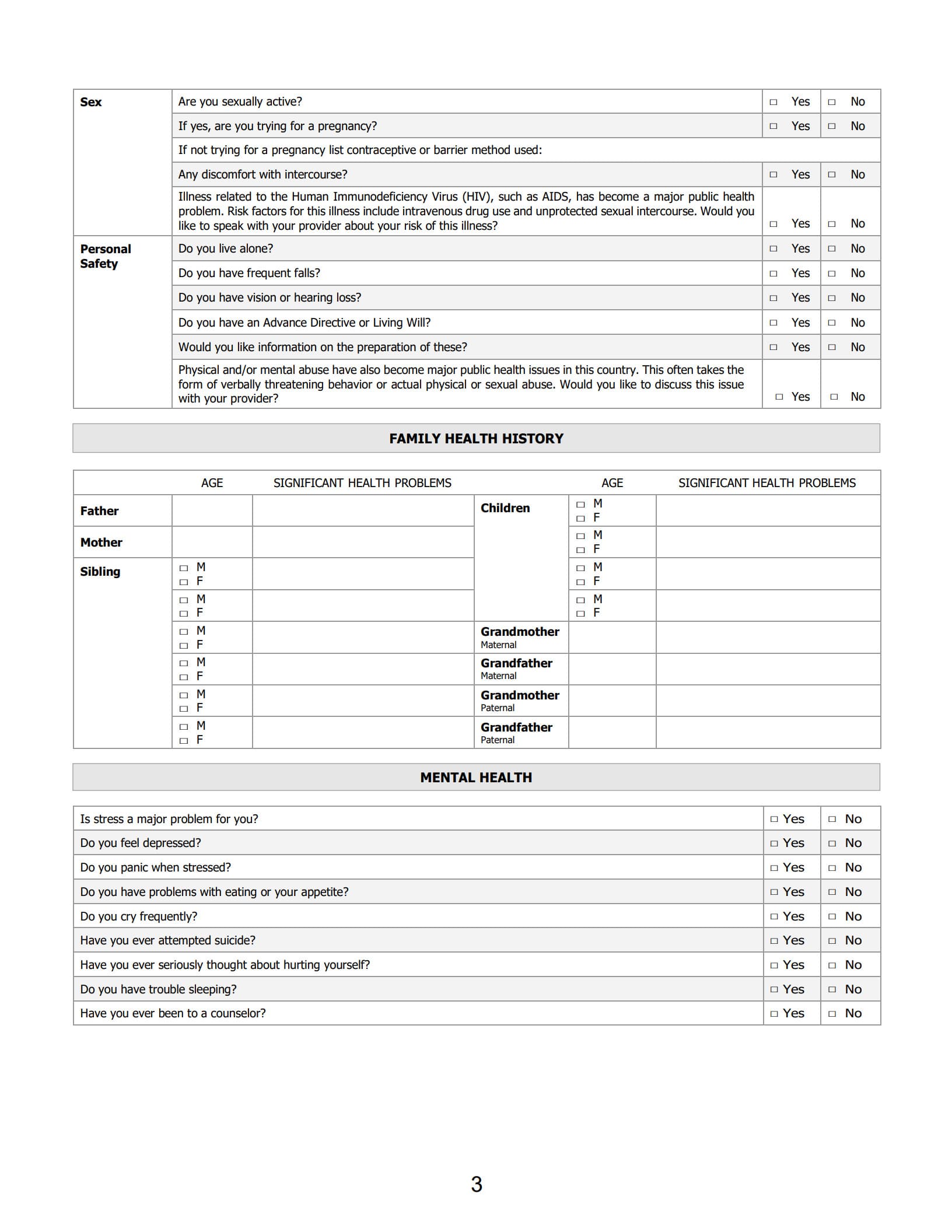
- Family History (FH): Documentation of the health status and causes of death of immediate relatives (parents, siblings, grandparents) to identify hereditary risks (e.g., heart disease, cancer, mental health issues).
- Personal and Social History: Information on lifestyle factors, including marital status, occupation, exercise habits, diet, alcohol use, tobacco use, and illicit drug use.
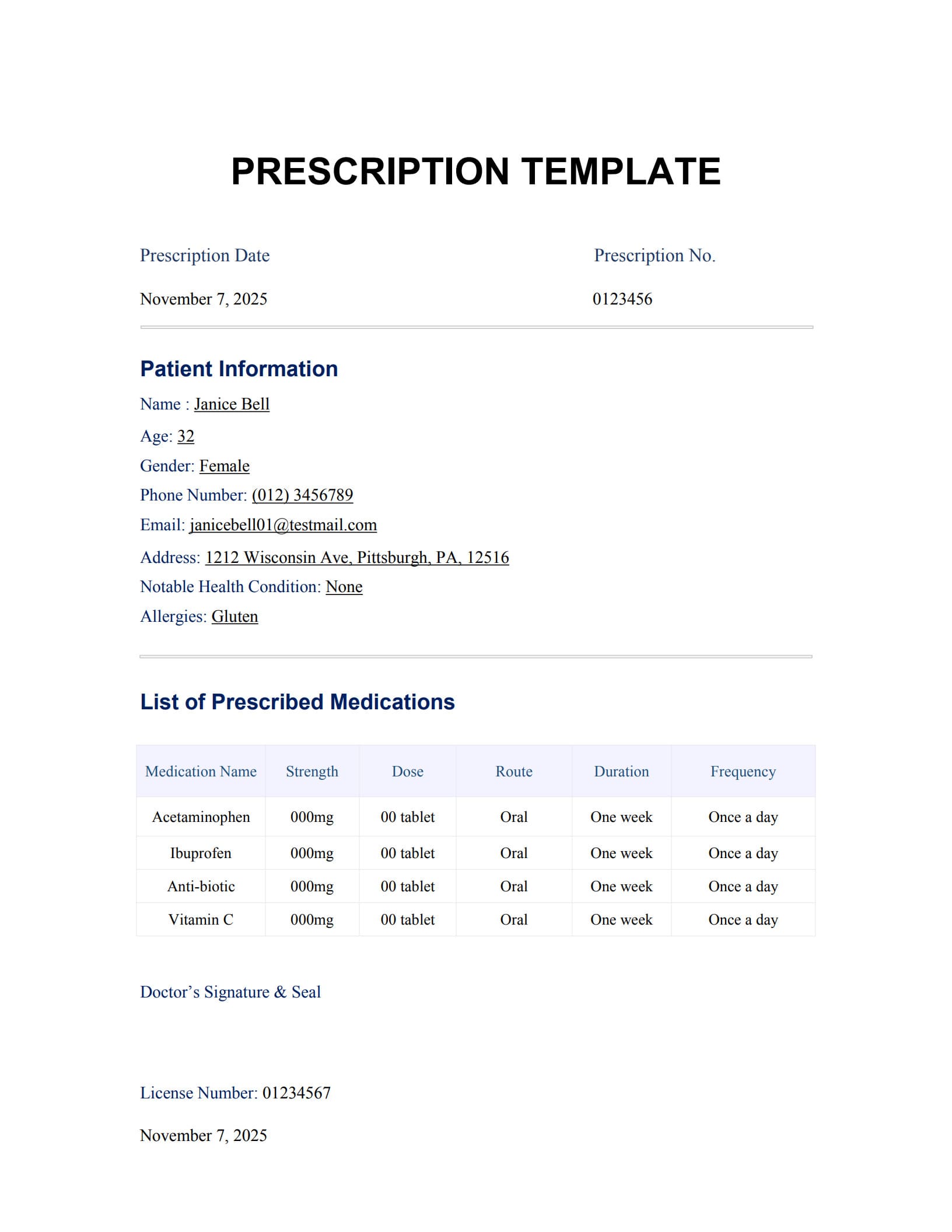
- Current Medications: A complete list of all prescriptions, over-the-counter drugs, vitamins, and herbal supplements, including dosage and frequency.
- Allergies: A list of all known allergies (medications, food, latex, etc.) and the specific reaction that occurred (e.g., rash, anaphylaxis).
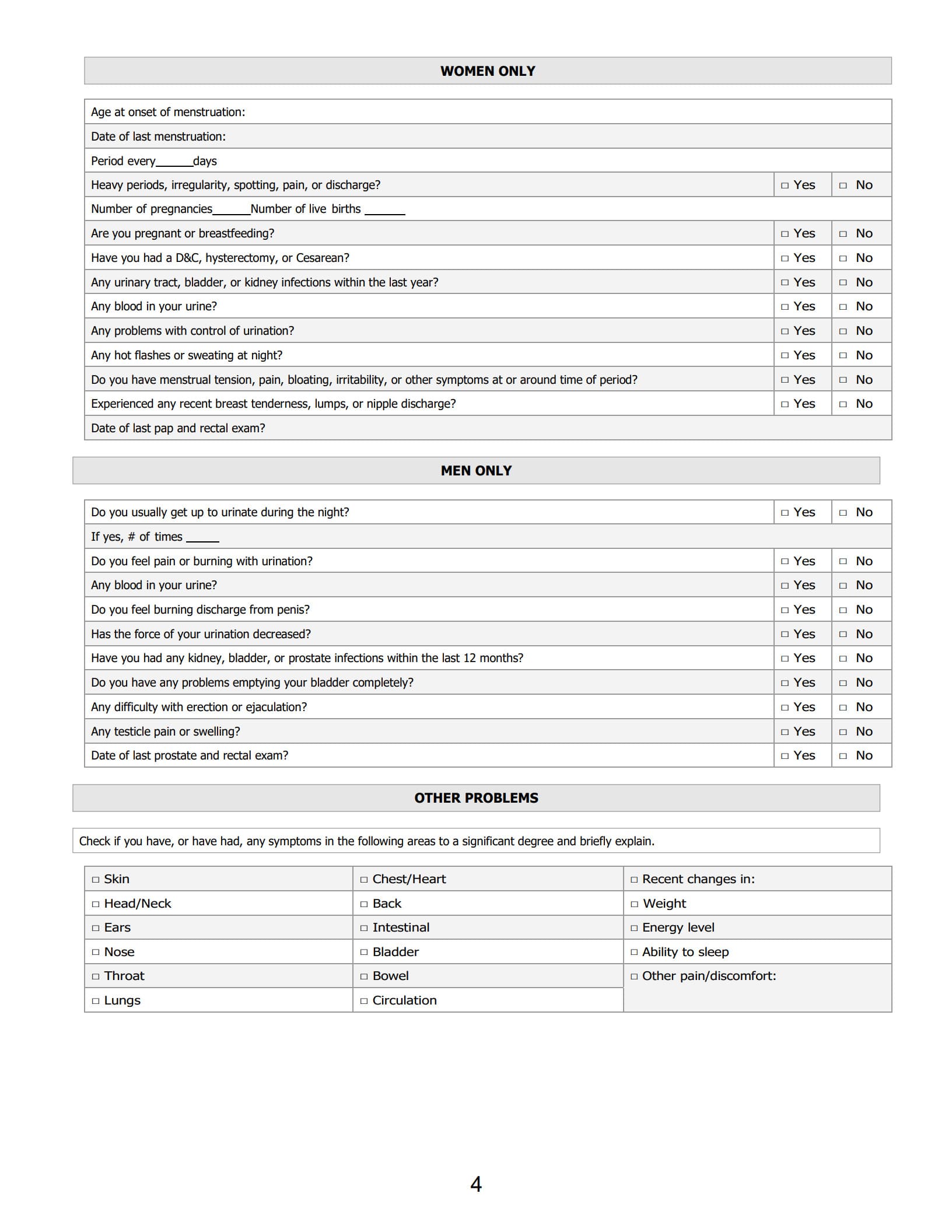
- Review of Systems (ROS): A systematic inventory of symptoms related to all body systems (e.g., cardiovascular, respiratory, gastrointestinal, neurological).
4. How to Complete a Medical History Form?
Whether you are the patient filling out the form or the medical assistant guiding the process, accuracy and completeness are crucial.
Tips for Patients to Complete a Health History Form:
- Be Thorough with Medications: Write down every medication, supplement, and vitamin, including the exact dosage. If you forget, take photos of the bottles.
- Be Precise with Allergies: Don't just list the medication; specify the reaction (e.g., "Penicillin – Hives/Swelling").
- Prioritize the Chief Complaint: Clearly explain why you are seeking care today, as this drives the physician's immediate focus.
Tips for Clinicians/Staff to Finish a Medical Record Template:
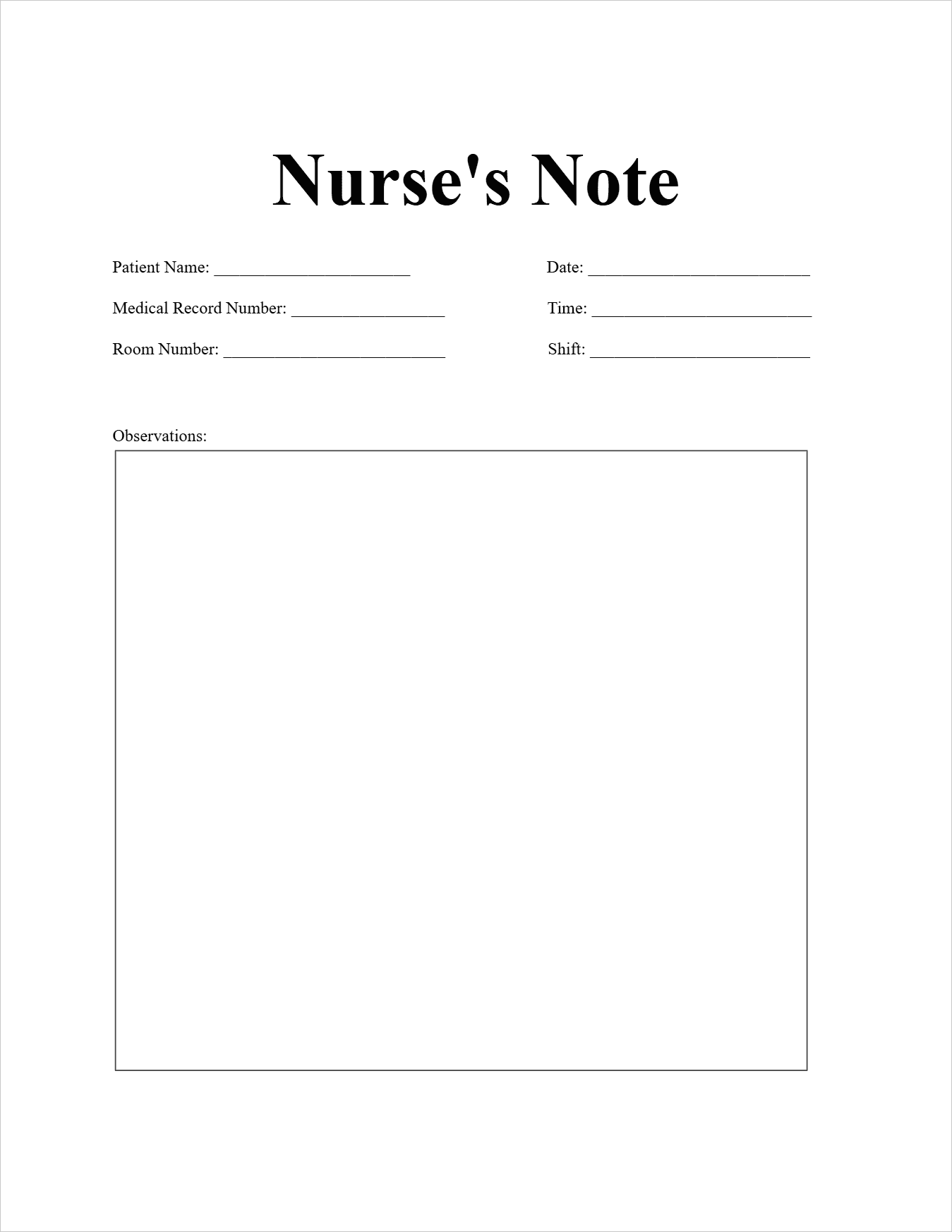
- Review Before the Provider: A Medical Assistant or Nurse should quickly review the form for major omissions (e.g., blank allergy section) and clarify any ambiguous patient handwriting before the physician enters the room.
- Use Open-Ended Questions: When clarifying the HPI, avoid leading questions. Ask "What makes the pain feel better?" rather than "Does Tylenol help?"
- Document Negative Findings: If the patient denies having a history of diabetes or denies any chest pain, document these denials explicitly in the record (e.g., "ROS: Denies chest pain or shortness of breath").
5. Customize with Health History Form Template
This template provides the essential structure for any comprehensive health history form.
Health History Form Template
| Section | Data Required | Example |
| I. PATIENT DEMOGRAPHICS | ||
| Full Name | [John A. Doe] | |
| DOB / Age | [01/01/1975] / [50] | |
| Emergency Contact | Name, Relationship, Phone | [Jane Doe, Spouse, 555-1234] |
| II. CHIEF COMPLAINT (CC) | The main reason for today's visit. | [Severe, throbbing headache for the last 3 days] |
| III. HISTORY OF PRESENT ILLNESS (HPI) | ||
| Onset | When did the problem start? | [Started Tuesday morning after exercise] |
| Location / Radiation | Where is the symptom located? Does it move? | [Left temporal region, does not radiate] |
| Severity (1-10) | Pain scale or degree of interference. | [Severity 8/10; makes it hard to focus at work] |
| Character | Describe the feeling (sharp, dull, throbbing). | [Throbbing, pulsating] |
| IV. PAST MEDICAL HISTORY (PMH) | ||
| Current Medications | Name, Dosage, Frequency | [Lisinopril 10 mg daily; Vitamin D 1000 IU daily] |
| Allergies & Reaction | Drug, Food, Environmental | [Penicillin (Anaphylaxis); Latex (Hives)] |
| Past Surgeries/Hospitalizations | Year and Reason | [Appendectomy 2005; Broken Leg 1998] |
| V. FAMILY HISTORY (FH) | ||
| Father's Health Status | [Deceased at 75 due to Myocardial Infarction] | |
| Mother's Health Status | [Living, Dx with Type 2 Diabetes] | |
| Siblings' Health Status | [One sister, healthy; One brother, high cholesterol] | |
| VI. SOCIAL HISTORY | ||
| Tobacco Use | Current, Former, or Never | [Former Smoker, Quit 10 years ago] |
| Alcohol Use | Frequency and Amount | [1-2 drinks per week (socially)] |
| Exercise/Diet | Frequency and Type | [Walks 30 mins, 5x/week; Balanced diet] |
6. FAQs about Health History Form Templates
6.1 What is an HPI form?
HPI stands for History of Present Illness. The HPI is the narrative or descriptive portion of the patient history that fully details the Chief Complaint (CC). It systematically explores the current problem using a structured format (like COLDSPA or PQRST) to gather comprehensive data on the symptoms, precipitating factors, duration, and attempts at self-treatment. It is not a separate form but a critical section within the overall Health History Form.
6.2 How to write a summary of medical history?
A summary of medical history should be a concise, chronological narrative focusing only on clinically significant events. It is often written at the beginning of a chart for quick review by any consulting physician.
Key components of a summary:
- Demographics & Diagnoses: Patient is a [Age] year old [Gender] with PMH of [List major active chronic conditions, e.g., hypertension, controlled asthma].
- Major Events: Note all major surgeries, hospitalizations, or serious injuries, including approximate dates.
- Allergies & Medications: State allergies (clearly mentioning the reaction) and list core current medications.
- Social Context: Briefly summarize key social factors (e.g., non-smoker, drinks socially, lives alone).
6.3 What are the guidelines for documenting the medical record?
Medical documentation must be accurate, legible, and timely to ensure patient safety and meet legal standards. Key guidelines include:
- Timeliness: Document notes immediately after the encounter or intervention. Late entries must be clearly labeled as such.
- Accuracy: Record all findings, interventions, and patient responses factually and objectively.
- Legibility: All entries must be readable (e-documentation is preferred). If handwritten, use blue or black ink.
- Authentication: All entries must be signed, dated, and timed by the person making the entry.
- Completeness: Ensure all questions and components of the history are addressed, even if the finding is "negative" (e.g., "Patient denies fever").
- No Erasures: Never erase, white-out, or completely obliterate an entry. Draw a single line through an error, write "Error" or "Mistaken Entry," and initial and date the correction.
Free Download: Printable Health History Form Template
You can download the Health History Form Template mentioned above by clicking the “Use Template” button on this page. Customize it to fit your specific needs and preferences.