Prescription writing is a core responsibility for authorized healthcare providers, requiring meticulous attention to detail to ensure patient safety and therapeutic efficacy. While digital tools have modernized the process (e-prescribing), understanding the foundational principles and standard formats remains crucial.
This guide explores the essential rules, terminology, and structure involved in safe and effective prescription writing, highlighting how prescription templates can standardize the process and minimize error.
1. What are the 7 Principles of Prescribing?
The principles of prescribing guide clinicians in making evidence-based, safe, and ethical choices for their patients. While the exact grouping may vary, the following seven principles are widely accepted globally:
- Diagnosis: Ensure the prescription is directly linked to an accurate, established diagnosis. Prescribe only when pharmacotherapy is genuinely indicated.
- Efficacy: Select a drug that has proven clinical effectiveness (efficacy) for the specific condition based on current, best-available evidence.
- Safety: Evaluate the potential for adverse effects, drug-drug interactions, contraindications (e.g., allergies, pregnancy), and patient risk factors (e.g., age, renal function).
- Suitability: Choose a dosage form, route, frequency, and duration that is appropriate for the individual patient’s needs, lifestyle, and ability to comply (e.g., liquid for a child, once-daily dosing for better adherence).
- Cost: Consider the overall cost to the patient and the healthcare system. Choose the most cost-effective option (e.g., generic over brand-name) without compromising safety or efficacy.
- Patient Education (Compliance): Clearly inform the patient about the medication's purpose, expected effects, common side effects, correct administration, storage, and when to seek follow-up care. Compliance is heavily reliant on understanding.
- Review and Monitoring: Plan for follow-up, ensuring the effectiveness and safety of the medication are monitored over time. Be ready to adjust or discontinue the drug if necessary.
2. The Most Frequent Terms in a Prescription
Prescriptions frequently use Latin abbreviations (or "Sig codes") to convey instructions quickly and universally. These codes are critical for pharmacists to accurately dispense the medication and for patients to understand the directions.
| Term/Abbreviation | Full Latin Term | Meaning |
| Rx | Recipe | Take, or preparation (The superscription) |
| Sig. | Signa | Let it be labeled (Directions for the patient) |
| q.d. | quaque die | Once daily (Avoid confusion; write "daily") |
| b.i.d. | bis in die | Twice daily |
| t.i.d. | ter in die | Three times daily |
| q.i.d. | quater in die | Four times daily |
| p.r.n. | pro re nata | As needed, or as the occasion arises |
| h.s. | hora somni | At bedtime |
| a.c. | ante cibum | Before meals |
| p.c. | post cibum | After meals |
| c | cum | With |
| s | sine | Without |
| stat | statim | Immediately |
| gtts | guttae | Drops |
3. What is the Best Way of Writing a Prescription?
Clarity is paramount in prescription writing. A poorly written or illegible prescription is a significant source of medication error.
Best Practices for Prescribing:
Legibility: If handwriting, print clearly and use capital letters for the drug name to avoid confusion (e.g., write "Levothyroxine" instead of "Levo..."). E-prescribing eliminates this issue entirely.
Completeness: Ensure all six parts (see FAQ 5.2) are present, especially patient identifiers and prescriber contact information.
Write the Indication: While not always mandatory, writing the reason for the medication (e.g., "for blood pressure") can help the pharmacist verify the appropriateness of the drug and help the patient remember its purpose.
Avoid Ambiguity: Always write out "daily" and "every other day" instead of using q.d. or q.o.d. Use metric units (mg, mL, g) and avoid apothecaries' units (grains, drams). Specify the dosage form (e.g., tablet, capsule, liquid).
Use Trailing Zeros Correctly: Never use a trailing zero (e.g., don't write "5.0 mg"). This can be misread as "50 mg." Always use a leading zero (e.g., write "0.5 mg").
Specify Quantity: Write the quantity in both numerals and words (e.g., "Quantity: 30 (thirty) tablets") to prevent alterations.
Refills: Clearly state the number of refills (e.g., "Refills: 3") or write "0" or "none."
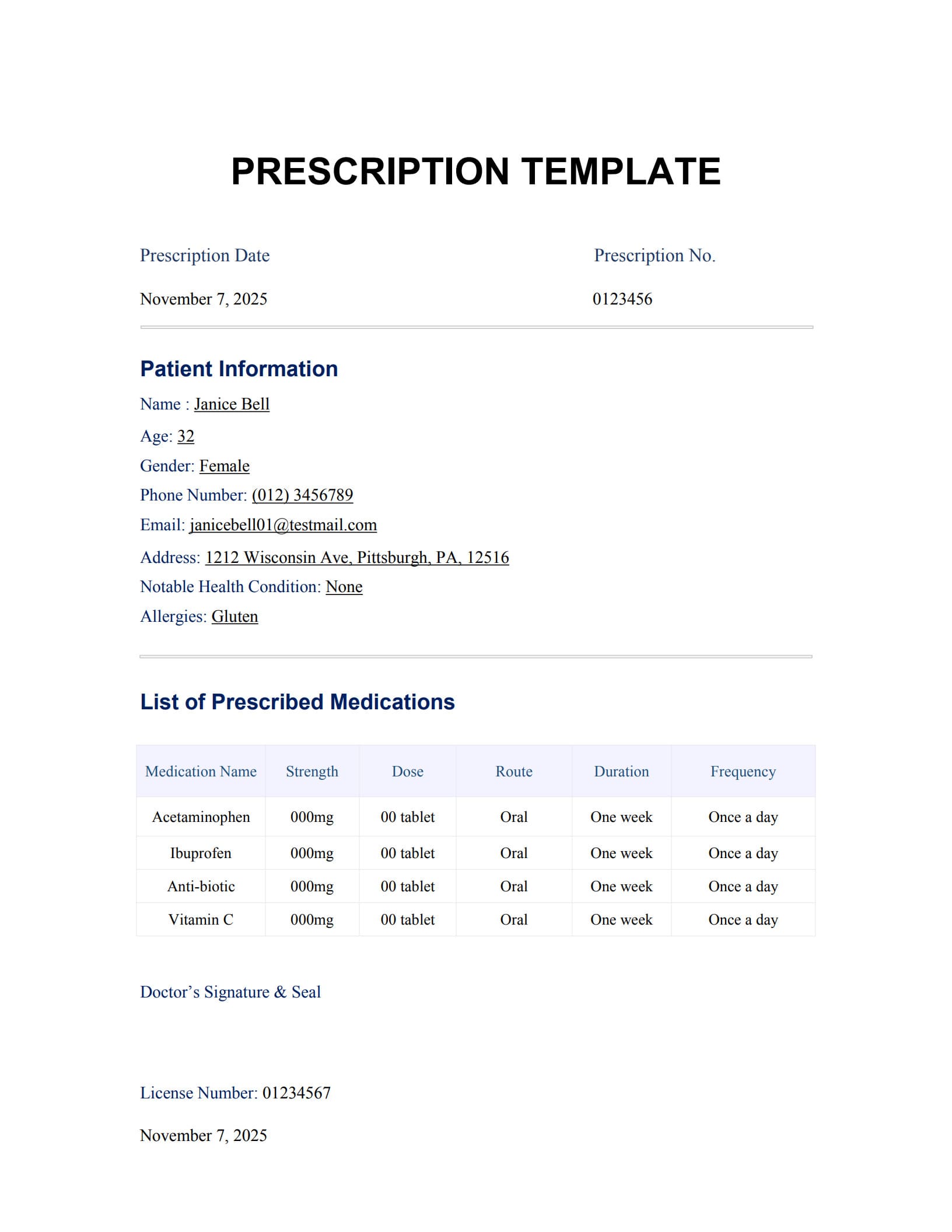
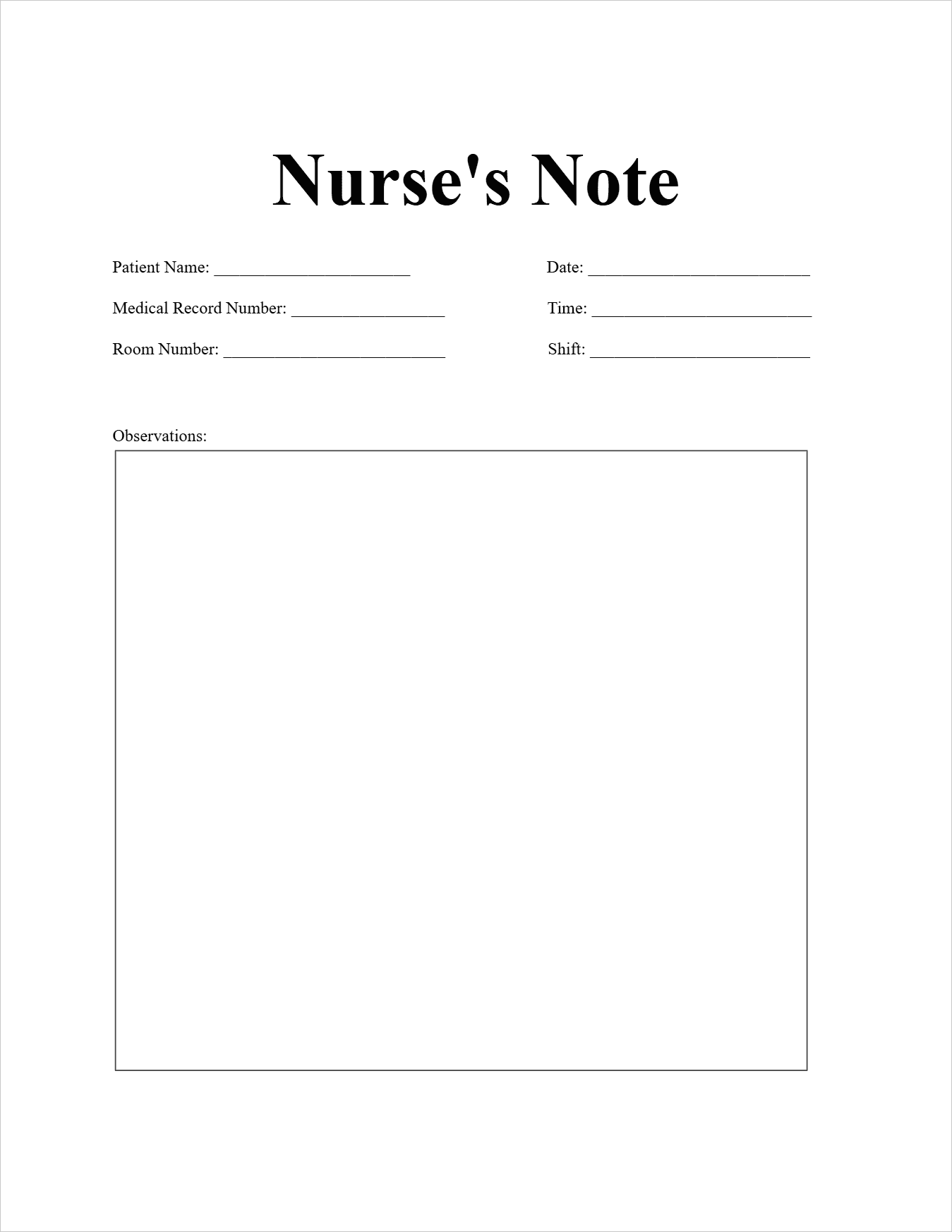
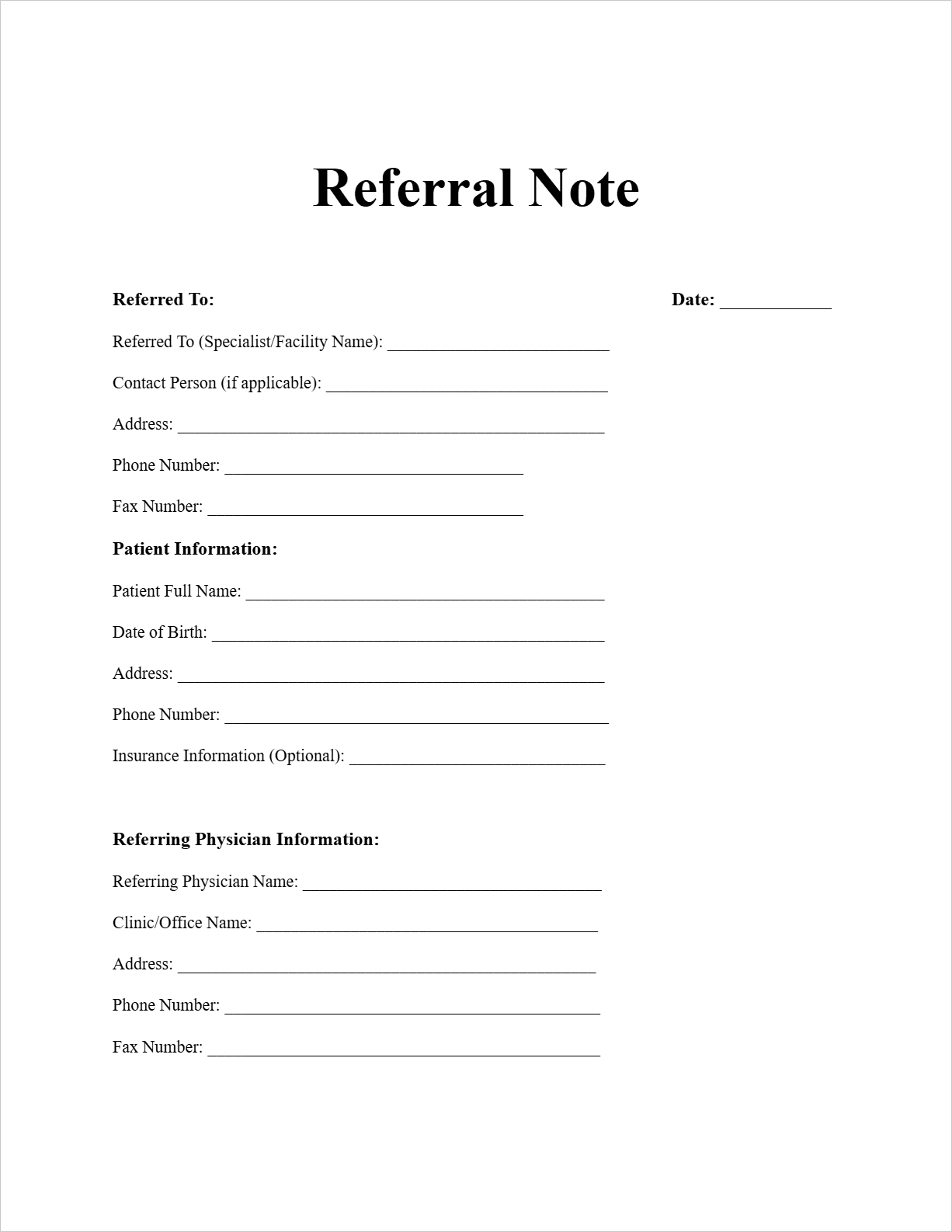
4. Quickly Get Started with a Prescription Template
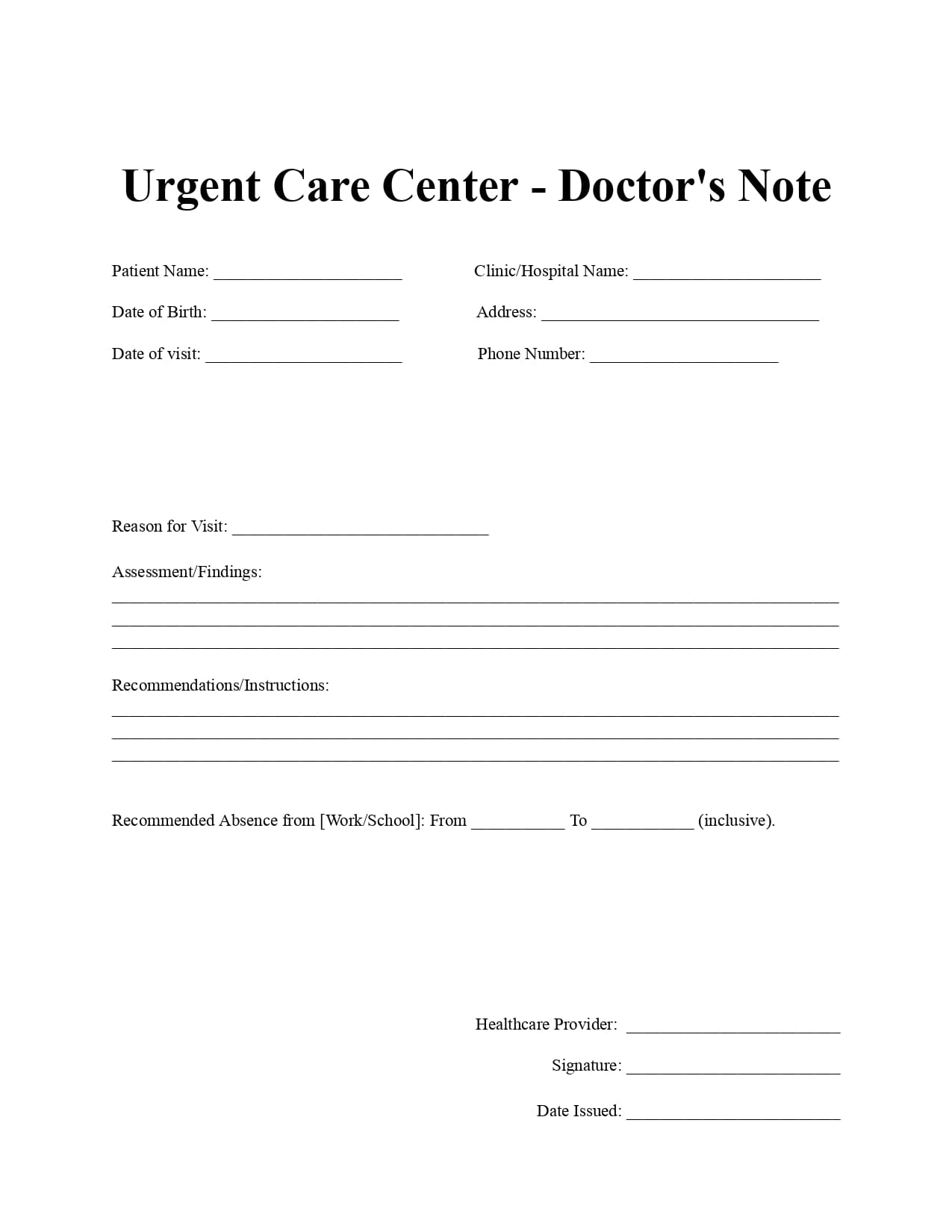
Prescription templates, especially in digital or PDF form, provide a standardized, pre-formatted document that ensures consistency and reduces the chance of skipping mandatory fields.
Benefits of Using a Free Editable Prescription Template:
- Standardization: Ensures every prescription contains the same required legal and medical fields, regardless of where the prescriber is located.
- Compliance: Built-in sections for NPI number, DEA number, and license information help meet regulatory requirements.
- Clarity: Dedicated spaces for patient demographics (DOB, address) prevent mixing up patient information.
- Error Reduction: Prompts and structured fields encourage the prescriber to specify drug form, quantity, and refills explicitly, mitigating common errors.
Rx Templates offer a reliable framework, making the process faster and safer, particularly for practitioners who still use paper prescriptions.
5. FAQs about Prescription Template
5.1 What is the Rx full form?
"Rx" is the abbreviation for prescription. The symbol Rx is traditionally considered an abbreviation for the Latin word Recipe, meaning "Take, thou." It serves as an instruction to the pharmacist to take the ingredients listed and prepare the medication.
5.2 What are the six parts of a written prescription order?
A complete written prescription order should contain the following six essential parts:
- Superscription: The patient's full name, address, date of birth (DOB), and the date the prescription was written.
- Inscription: The name of the drug, the dosage form (e.g., tablet), and the strength (e.g., 50 mg).
- Subscription: The dispensing instructions to the pharmacist, often specifying the total quantity to be dispensed (e.g., Disp. #30).
- Signatura (Sig.): The directions for the patient, including the route of administration, frequency, and duration (e.g., "Take 1 tablet by mouth twice daily").
- Refill Information: The number of authorized refills (e.g., "Refills: 2" or "0").
- Prescriber Information: The prescriber's name, professional credentials, signature, and necessary identification numbers (e.g., NPI, DEA).
5.3 How long does a prescription sheet last?
The validity of a prescription sheet (meaning the time frame within which it must be filled for the first time) varies significantly by country, state, and the class of drug:
- Non-Controlled Substances: Often valid for up to 6 months to 1 year from the date it was written.
- Controlled Substances (e.g., Schedule II/III/IV): Typically have much shorter validity, often 7, 30, or 90 days, and may have restrictions on the number of days' supply.
Always check local and federal regulations, as the rules for controlled substances are the strictest and most prone to change.
5.4 What is the most common prescribing error?
The most common prescribing errors often revolve around dosing and frequency. Specific frequent errors include:
- Dose Confusion: Mistaking strength (e.g., 0.5 mg vs. 5 mg).
- Ambiguous Instructions: Using unapproved abbreviations (e.g., "u" for units, which can look like a "0").
- Incomplete Directions: Failure to specify the duration of therapy or the maximum daily dose for PRN (as-needed) medications.
Inappropriate Drug Selection: Prescribing a medication to which the patient is allergic or which significantly interacts with another current medication.
Free Download: Printable Prescription Template
You can download the Prescription Template mentioned above by clicking “Use Template” button on this page. Customize it to fit your specific needs and preferences.