Nurses are at the forefront of patient care, constantly monitoring conditions, administering treatments, and providing compassionate support. Accurate and comprehensive documentation is a cornerstone of their practice, ensuring seamless communication among the healthcare team and the delivery of safe and effective care. Nursing notes serve as this vital record, capturing the nuances of a patient's status and the interventions provided. This article will delve into the importance of nursing notes, explore their differences from nursing charts, highlight various use cases, and provide a practical example using our Nursing Note template.
What are Nursing Notes?
Nursing notes are detailed records created by nurses to document their observations, the care they provide, the patient's response to treatment, and any communication with other healthcare team members or the patient's family. These notes are an integral part of the patient's medical record and provide a chronological account of the nursing care delivered throughout a nurse's shift. They offer valuable insights into the patient's condition, progress, and overall well-being, contributing significantly to informed decision-making and continuity of care.
Differences between Nursing Notes and Nursing Charts
While the terms are sometimes used interchangeably, there's a subtle distinction between nursing notes and nursing charts:
- Nursing Notes: These are the narrative, written entries made by nurses to document specific observations, interventions, and patient responses during their shift. They provide a detailed account of the care provided and the patient's status at various points in time. The template we are focusing on is for these detailed, shift-by-shift entries.
- Nursing Charts (or Flow Sheets): These are typically more structured documents or sections within the electronic health record used to record routine data in a standardized format. This includes vital signs, medication administration records, intake and output measurements, and other quantifiable data. Charts often use tables and predefined fields for efficiency.
Think of nursing notes as the qualitative, descriptive record, while nursing charts are more quantitative and tabular. Both are essential components of the overall nursing documentation.
Nursing Notes Use Cases
Nursing notes are fundamental to the delivery of safe and effective patient care, serving a multitude of critical purposes across diverse healthcare settings:
Documenting Patient Assessments (Foundation of Care Planning):
This use case forms the bedrock of individualized nursing care. Nurses perform comprehensive assessments upon a patient's arrival and continuously throughout their stay. Detailed nursing notes capture these assessments, including vital signs, physical findings (such as skin integrity, respiratory effort, bowel sounds), mental status (level of consciousness, orientation), emotional state (mood, affect, anxiety levels), pain levels and characteristics, and functional abilities (mobility, ability to perform activities of daily living). This information isn't just data points; it forms the basis for identifying patient needs, developing individualized care plans, and recognizing any changes or trends in their condition. For example, a nurse might document a patient's initial assessment revealing decreased breath sounds and a productive cough, which would contribute to a nursing diagnosis of impaired gas exchange and guide subsequent interventions.
Detailing Interventions (A Record of Care Provided):
Nursing notes meticulously record all the nursing care provided to the patient. This includes the administration of medications (route, dosage, time, and any pre-assessment or patient teaching), wound care procedures (dressing changes, assessment of wound appearance), implementation of treatments (such as oxygen therapy, catheter care, application of restraints), patient education (topics covered, patient's understanding), and assistance with activities of daily living (hygiene, feeding, ambulation). This detailed record ensures that all ordered care is delivered and provides a clear picture of the nursing actions taken. For instance, a note might detail the steps taken during a complex dressing change for a surgical wound, including the type of dressing used, the condition of the wound bed, and the patient's tolerance of the procedure.
Tracking Patient Responses (Monitoring Effectiveness of Care):
Simply providing care isn't enough; nurses must also document how the patient responds to interventions. Nursing notes capture these responses, whether positive or negative. This includes the patient's reaction to medications (pain relief, side effects), tolerance of treatments (e.g., how well they tolerated a physical therapy session), changes in symptoms after interventions (e.g., decreased shortness of breath after oxygen administration), and overall progress towards goals. This ongoing evaluation, documented in the notes, allows the healthcare team to assess the effectiveness of the care plan and make necessary adjustments. An example would be a nurse noting that the patient reported a significant decrease in pain 30 minutes after receiving pain medication.
Recording Communication (Ensuring Team Collaboration):
Effective communication among all members of the healthcare team is paramount for coordinated and safe patient care. Nursing notes serve as a critical communication tool, documenting any interactions with physicians (e.g., notification of changes in patient condition, clarification of orders), other nurses (e.g., information shared during shift handovers), therapists (e.g., patient's progress reported by physical therapy), the patient, and their family members (e.g., updates provided, concerns discussed). This ensures that everyone involved in the patient's care is aware of relevant information and can contribute to a unified approach. A nurse might note a phone conversation with the physician regarding a patient's elevated blood pressure and the subsequent orders received.
Updating the Plan of Care (Reflecting Evolving Needs):
The patient's condition and needs can change rapidly. Nursing notes play a vital role in documenting any modifications or updates to the patient's nursing care plan. Based on ongoing assessments and the patient's response to interventions, nurses will document any adjustments made to address new issues or evolving needs. This ensures that the care plan remains relevant and tailored to the patient's current situation. For example, if a patient's mobility decreases, the nursing note might reflect an update to the care plan to include increased assistance with ambulation and fall precautions.
Providing Legal Documentation (Protecting Patients and Professionals):
Nursing notes are legal documents that serve as a comprehensive record of the care provided. In the event of any legal inquiries or quality reviews, these notes provide evidence of the assessments performed, the interventions implemented, and the patient's outcomes. Accurate, complete, and timely nursing notes are essential for protecting both the patient's rights and the nurse's professional integrity. Clear and factual documentation can be crucial in demonstrating the standard of care provided.
Facilitating Shift Handovers (Ensuring Continuity and Safety):
At the end of each nursing shift, a thorough handover report is essential to ensure a smooth transition of care to the oncoming nurse. Nursing notes provide the vital information needed for an effective handover, summarizing the patient's current status, any significant events that occurred during the shift, ongoing interventions, and any anticipated needs or concerns for the next shift. This promotes continuity of care and helps prevent errors or omissions. A well-written nursing note allows the next nurse to quickly understand the patient's situation and prioritize their care effectively.
In summary, nursing notes are much more than just scribbles on a chart. They are a dynamic and indispensable tool that underpins safe, effective, and patient-centered care. They serve as a detailed account of the nursing process in action, reflecting the continuous assessment, planning, implementation, and evaluation that are the hallmarks of professional nursing practice.
Nursing Note Example
Let's revisit our patient, Alice Johnson, and see how a nurse named Maria Rodriguez documented her care during a day shift:
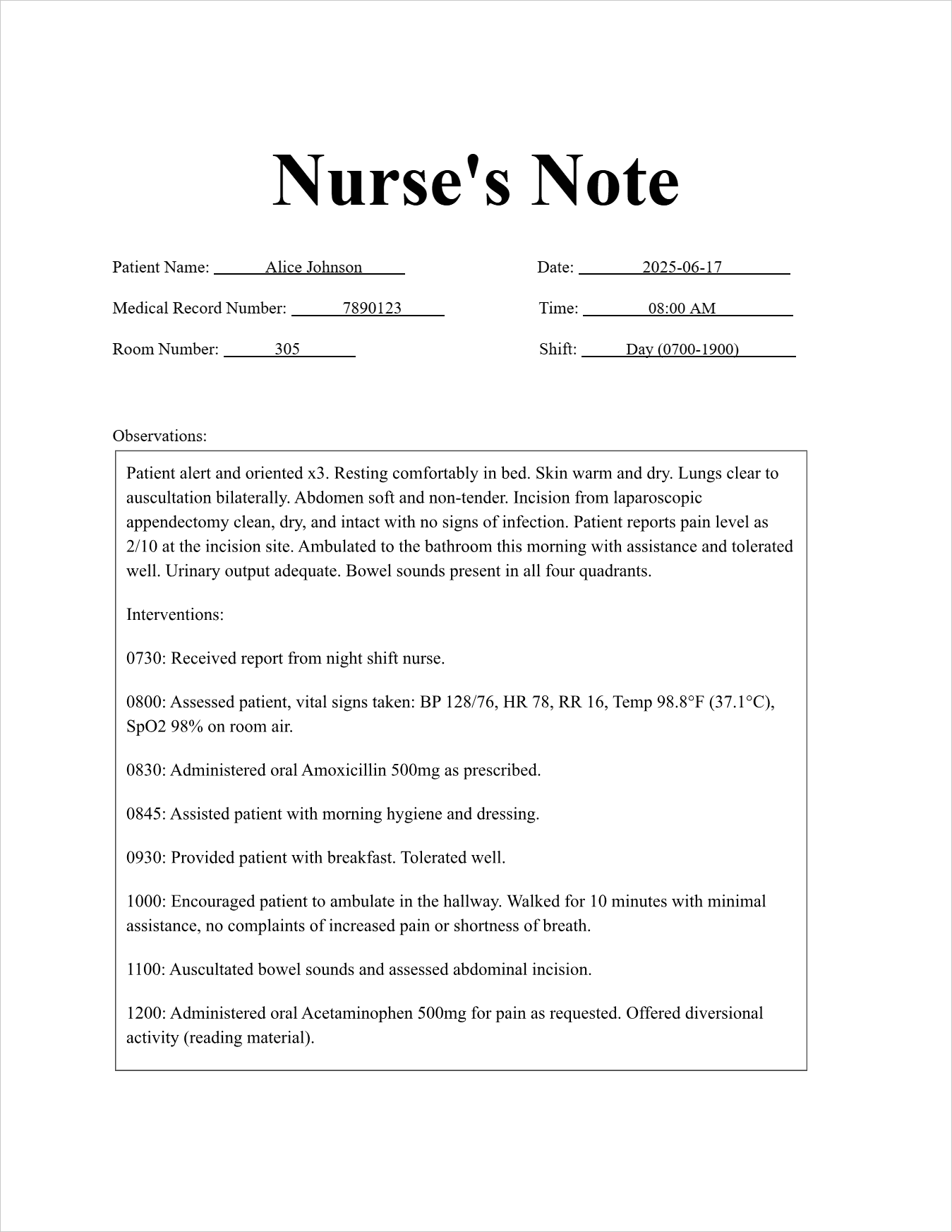
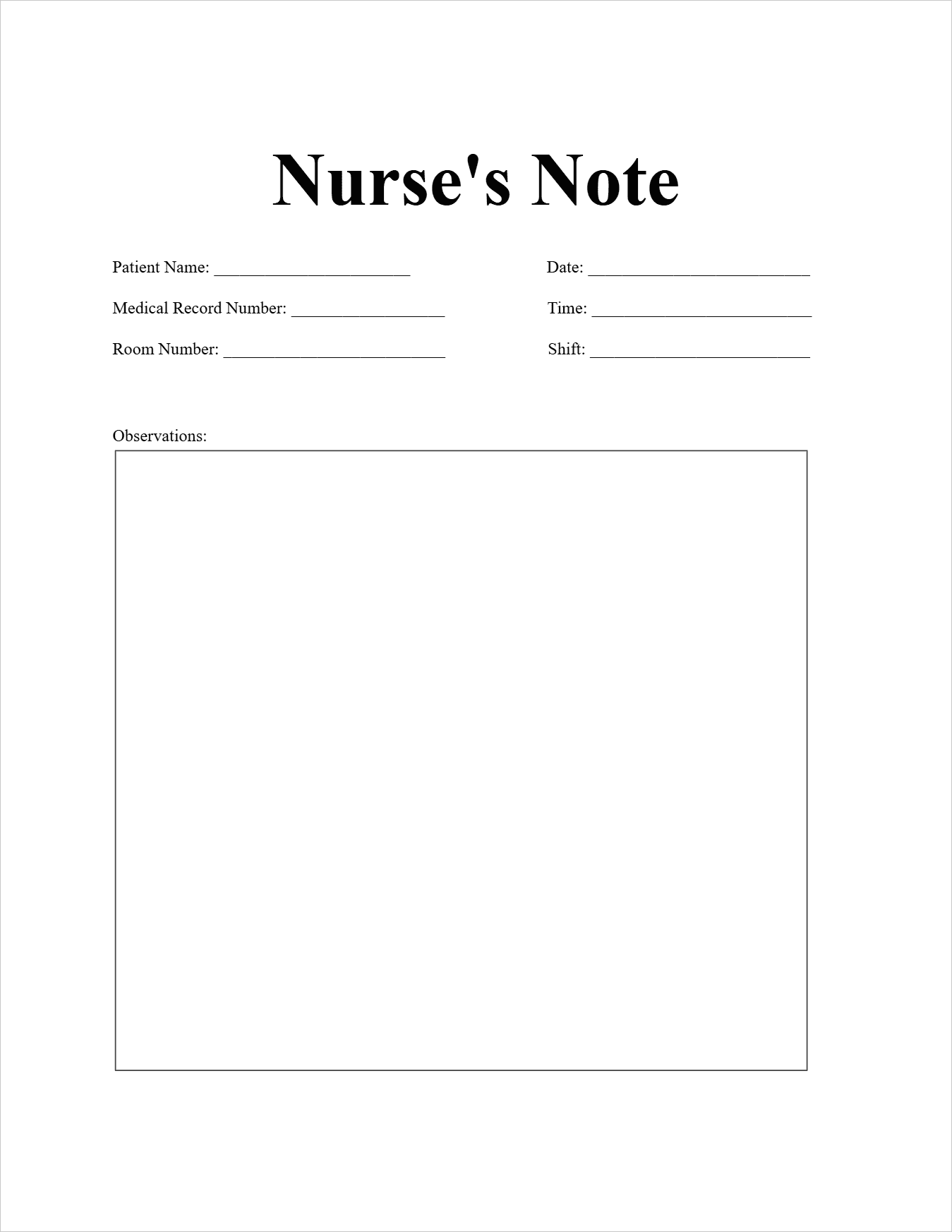
Nurse's Note
Patient Information:
Patient Name: Alice Johnson
Medical Record Number: 7890123
Room Number: 305
Date and Time:
Date: 2025-06-17
Time: 08:00 AM
Shift: Day (0700-1900)
Observations: Patient alert and oriented x3. Resting comfortably in bed. Skin warm and dry. Lungs clear to auscultation bilaterally. Abdomen soft and non-tender. Incision from laparoscopic appendectomy clean, dry, and intact with no signs of infection. Patient reports pain level as 2/10 at the incision site. Ambulated to the bathroom this morning with assistance and tolerated well. Urinary output adequate. Bowel sounds present in all four quadrants.
Interventions:
0730: Received report from night shift nurse.
0800: Assessed patient, vital signs taken: BP 128/76, HR 78, RR 16, Temp 98.8°F (37.1°C), SpO2 98% on room air.
0830: Administered oral Amoxicillin 500mg as prescribed.
0845: Assisted patient with morning hygiene and dressing.
0930: Provided patient with breakfast. Tolerated well.
1000: Encouraged patient to ambulate in the hallway. Walked for 10 minutes with minimal assistance, no complaints of increased pain or shortness of breath.
1100: Auscultated bowel sounds and assessed abdominal incision.
1200: Administered oral Acetaminophen 500mg for pain as requested. Offered diversional activity (reading material).
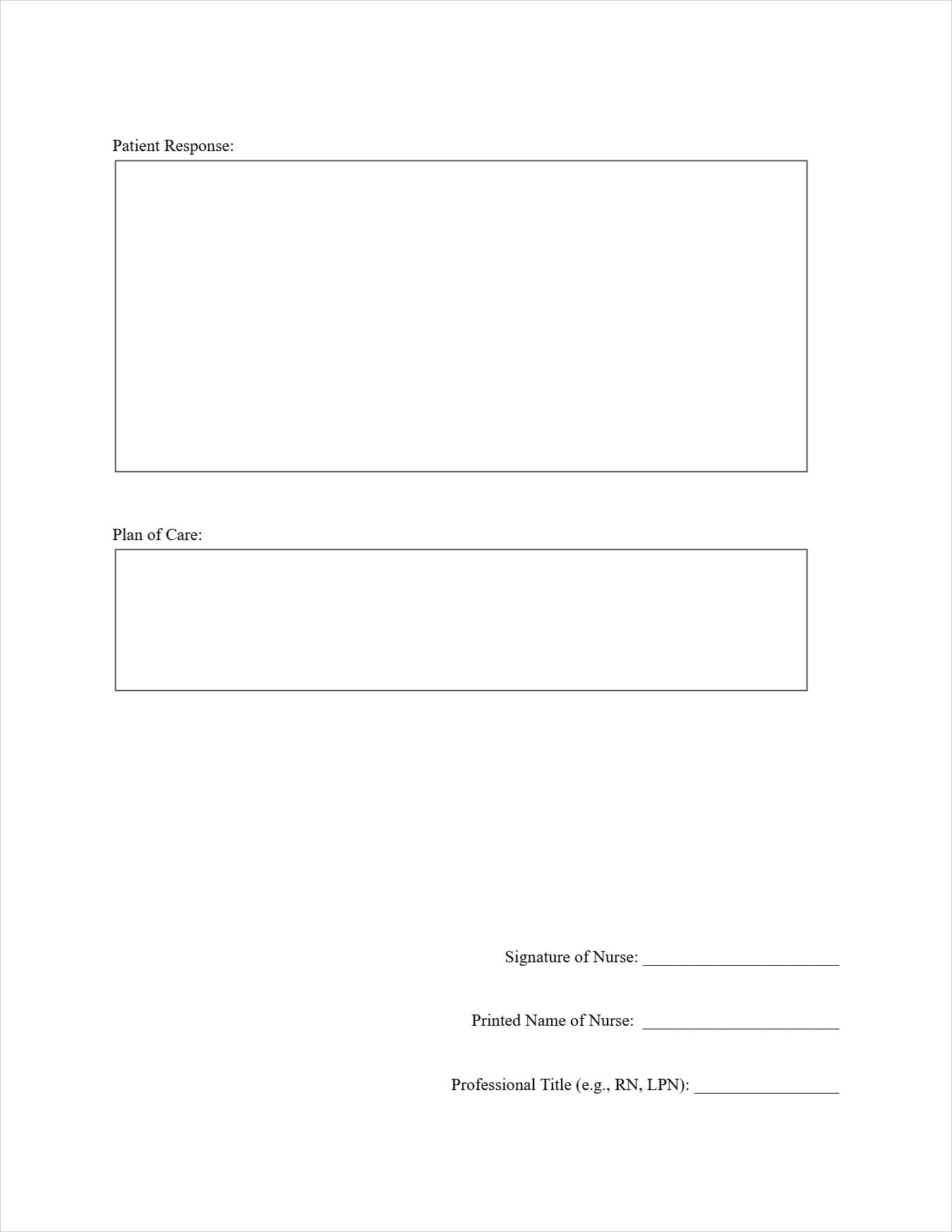
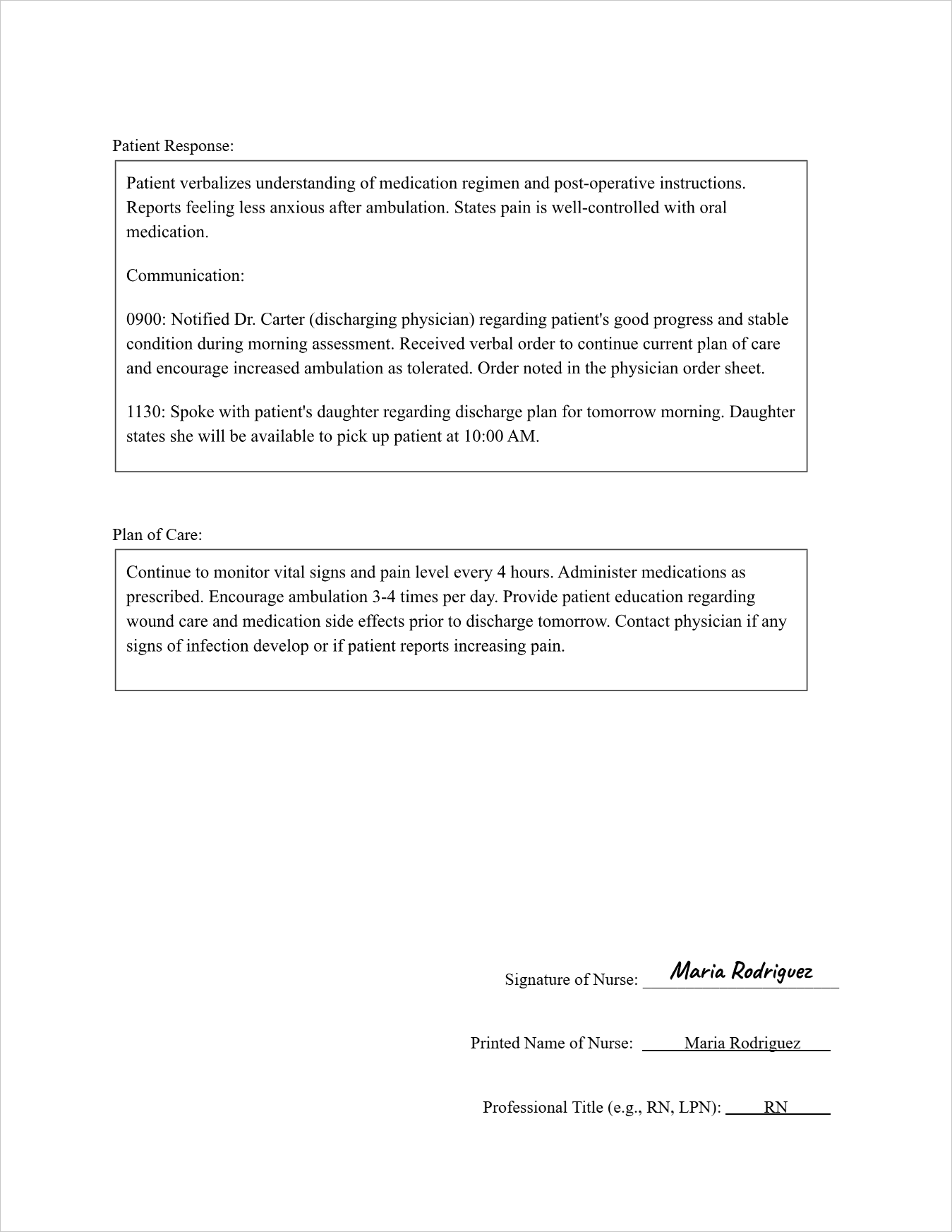
Patient Response: Patient verbalizes understanding of medication regimen and post-operative instructions. Reports feeling less anxious after ambulation. States pain is well-controlled with oral medication.
Communication:
0900: Notified Dr. Carter (discharging physician) regarding patient's good progress and stable condition during morning assessment. Received verbal order to continue current plan of care and encourage increased ambulation as tolerated. Order noted in the physician order sheet.
1130: Spoke with patient's daughter regarding discharge plan for tomorrow morning. Daughter states she will be available to pick up patient at 10:00 AM.
Plan of Care: Continue to monitor vital signs and pain level every 4 hours. Administer medications as prescribed. Encourage ambulation 3-4 times per day. Provide patient education regarding wound care and medication side effects prior to discharge tomorrow. Contact physician if any signs of infection develop or if patient reports increasing pain.
Signature of Nurse: (Imagine a signature is drawn here)
Printed Name of Nurse: Maria Rodriguez
Professional Title (e.g., RN, LPN): RN
FAQs about the Nursing Note Template
What abbreviations are commonly used in nursing notes?
Nurses often use standardized medical abbreviations to save time and space while ensuring clarity. Examples include VS (vital signs), HR (heart rate), BP (blood pressure), RR (respiratory rate), Temp (temperature), SpO2 (oxygen saturation), RA (room air), CDI (clean, dry, intact), BR (bathroom), UO (urinary output), BS (bowel sounds), PO (by mouth), q4h (every 4 hours), TID (three times a day), and MD (medical doctor).
How often should nursing notes be written?
Nursing notes are typically documented after each significant interaction with the patient or at least once per shift, depending on the patient's condition and the facility's policies.
What should be avoided in nursing notes?
Subjective opinions, personal biases, and blaming language should be avoided. Notes should be factual, objective, and focused on the patient's condition and care provided.
Are nursing notes legal documents?
Yes, nursing notes are legal documents and can be used as evidence in legal proceedings. Therefore, accuracy, completeness, and timeliness are crucial.
How have electronic health records (EHRs) impacted nursing notes?
EHRs have significantly changed nursing documentation, often incorporating standardized templates, drop-down menus, and electronic signatures. While the format might differ, the core principles of accurate and comprehensive documentation remain the same.
Free Download: Printable Nursing Note Template
You can download the Nursing Note Template mentioned above by clicking Use Template button on this page. Customize it to fit your specific needs and preferences.