Effective collaboration and communication among healthcare professionals are crucial for providing the best possible patient care. When a primary care physician seeks the expertise of a specialist, a consultation note serves as a vital record of this interaction. It documents the reason for the consultation, the information shared, the specialist's findings and assessment, and their recommendations for the patient's ongoing care. This article will explore the importance of consultation notes and provide a practical example using our Consultation Note template.
What are Consultation Notes?
Consultation notes are formal medical documents that record the interaction between a requesting healthcare provider (often a primary care physician) and a consulting healthcare provider (typically a specialist). The purpose of a consultation is to obtain expert advice or guidance on a patient's specific medical condition or treatment plan. The consultation note summarizes the reason for the request, the relevant patient history, the consulting provider's examination findings, their assessment of the patient's condition, and their specific recommendations for diagnosis, treatment, or management. These notes facilitate clear communication and ensure a coordinated approach to patient care.
Consultation Note Example
Imagine Dr. Susan Lee, a primary care physician, reached out to Dr. Michael Brown, a cardiologist, for advice regarding her patient, Robert Garcia. Here’s how their consultation would be documented using our template:
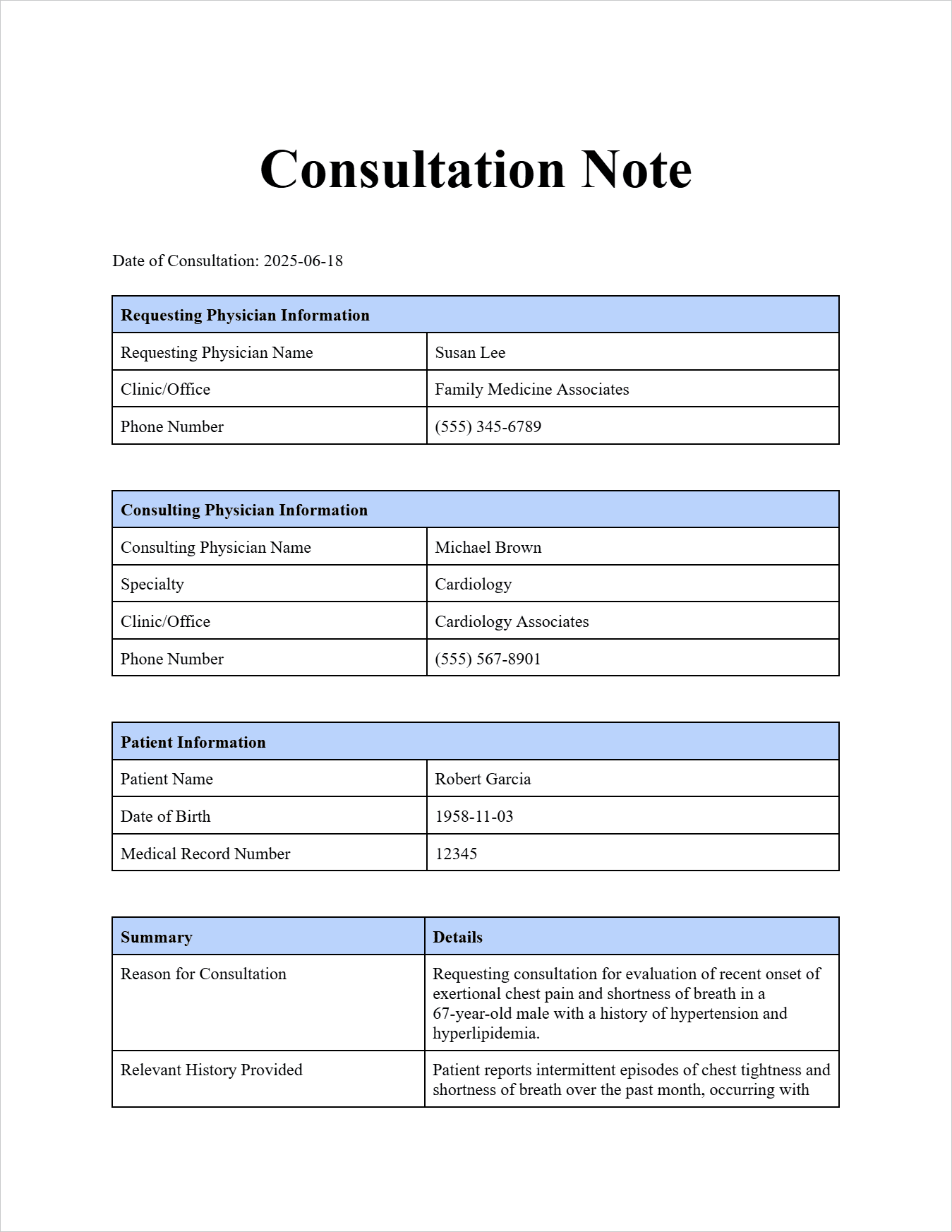
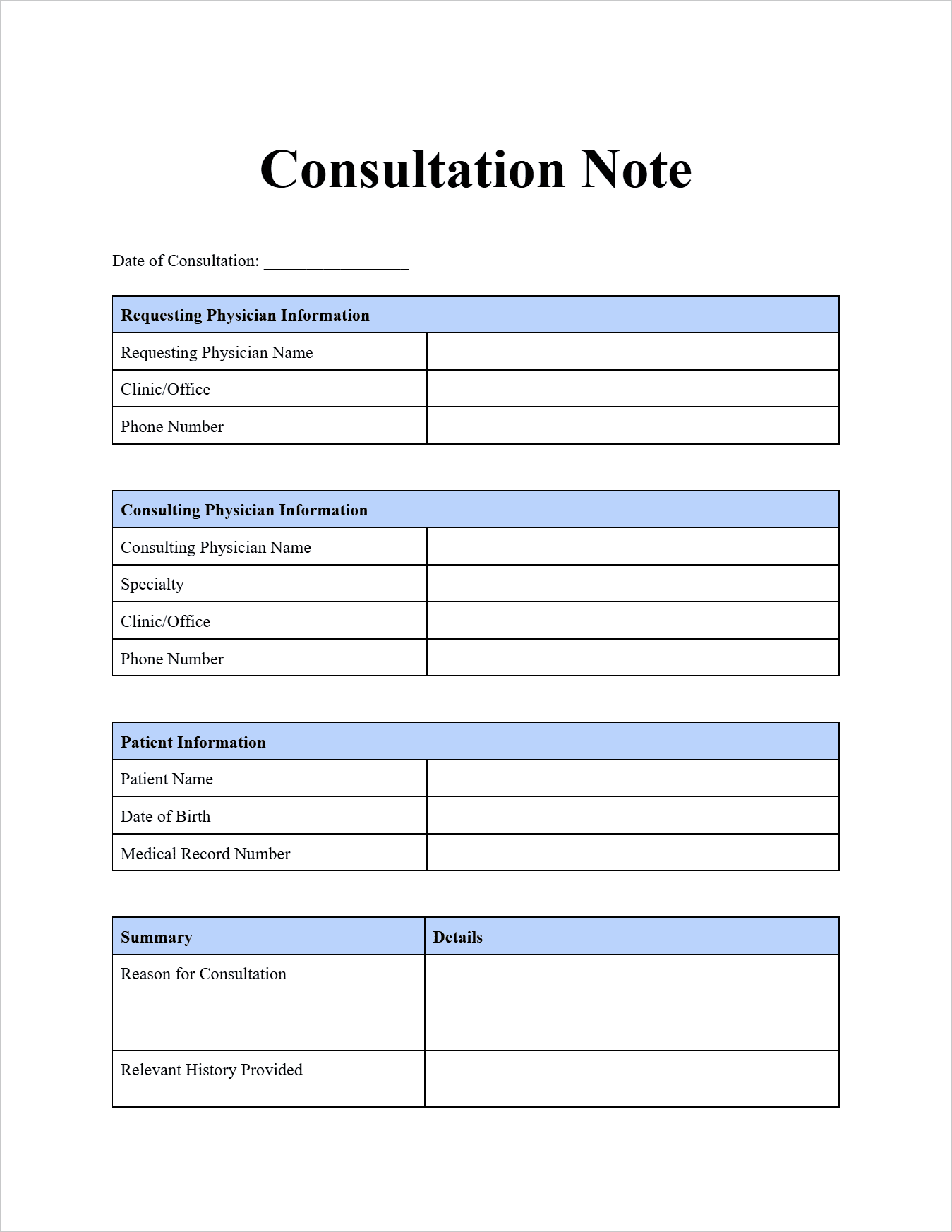
Consultation Note
Requesting Physician Information:
Requesting Physician Name: Susan Lee
Clinic/Office: Family Medicine Associates
Phone Number: (555) 345-6789
Consulting Physician Information:
Consulting Physician Name: Michael Brown
Specialty: Cardiology
Clinic/Office: Cardiology Associates
Phone Number: (555) 567-8901
Patient Information:
Patient Name: Robert Garcia
Date of Birth: 1958-11-03
Medical Record Number: 12345
Date of Consultation: 2025-06-18
Reason for Consultation: Requesting consultation for evaluation of recent onset of exertional chest pain and shortness of breath in a 67-year-old male with a history of hypertension and hyperlipidemia.
Relevant History Provided: Patient reports intermittent episodes of chest tightness and shortness of breath over the past month, occurring with moderate exertion and relieved by rest. Episodes last for approximately 5-10 minutes. He denies any associated radiation of pain, diaphoresis, or nausea. Resting ECG performed in our office today showed no acute ST-T wave changes.
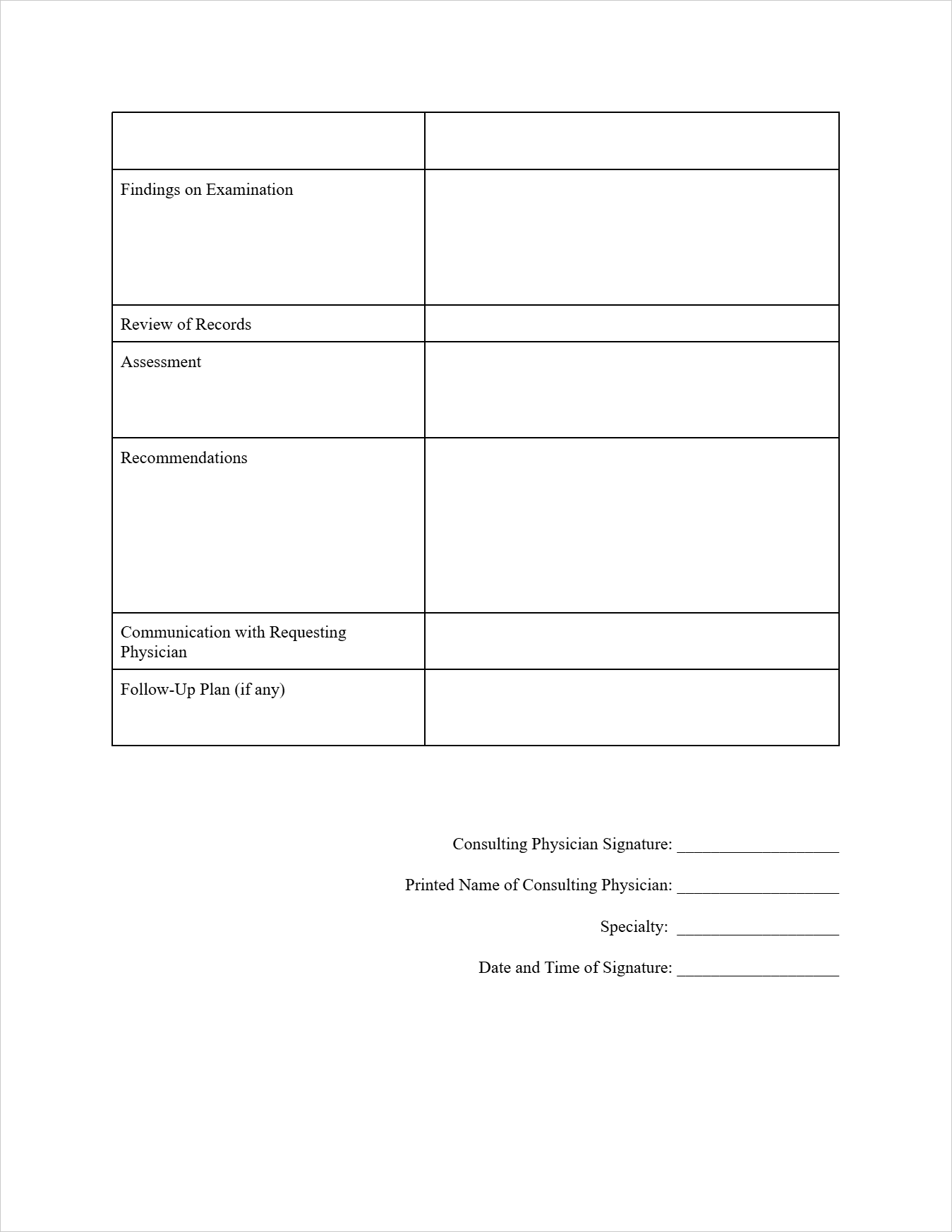
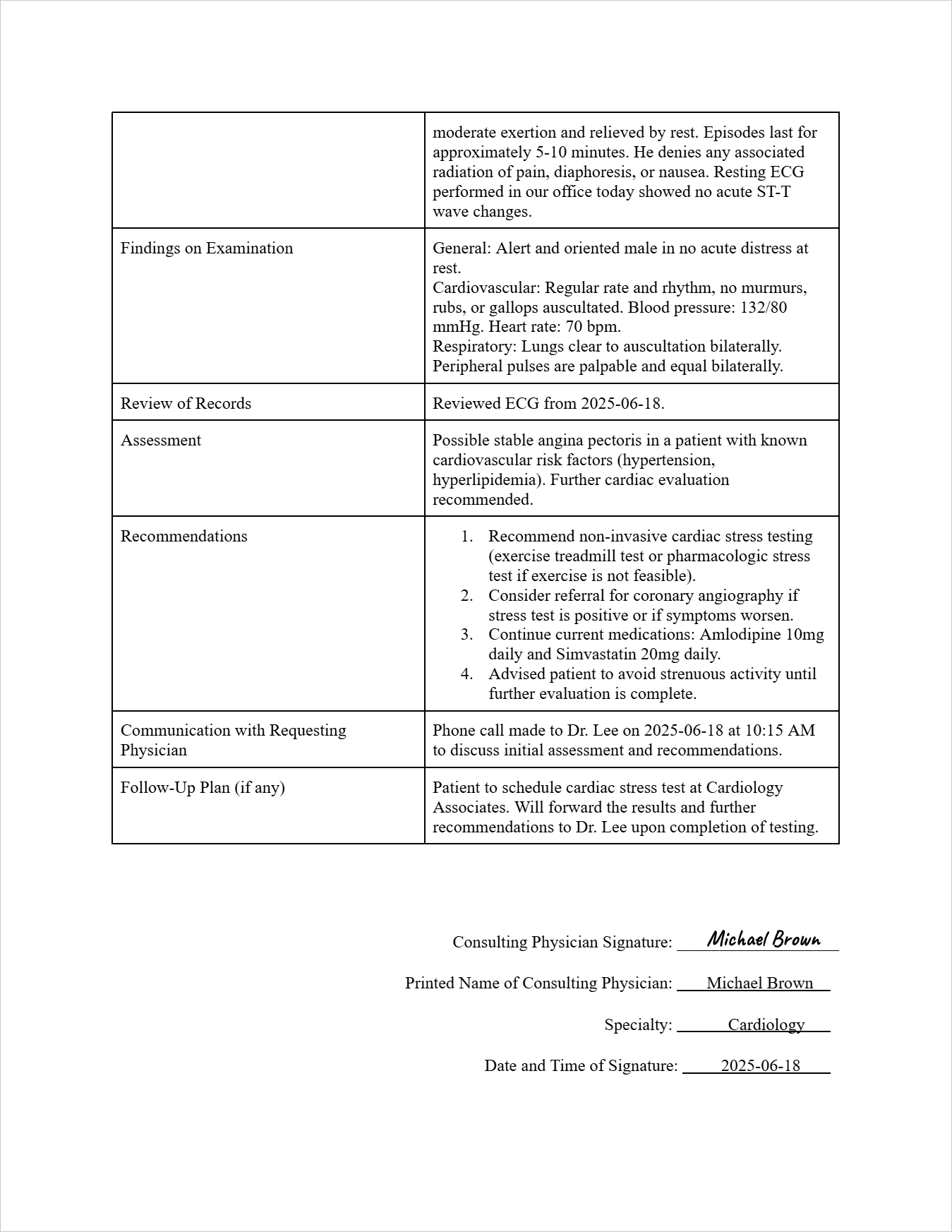
Findings on Examination:
General: Alert and oriented male in no acute distress at rest.
Cardiovascular: Regular rate and rhythm, no murmurs, rubs, or gallops auscultated. Blood pressure: 132/80 mmHg. Heart rate: 70 bpm.
Respiratory: Lungs clear to auscultation bilaterally.
Peripheral pulses are palpable and equal bilaterally.
Review of Records: Reviewed ECG from 2025-06-18.
Assessment: Possible stable angina pectoris in a patient with known cardiovascular risk factors (hypertension, hyperlipidemia). Further cardiac evaluation recommended.
Recommendations:
- Recommend non-invasive cardiac stress testing (exercise treadmill test or pharmacologic stress test if exercise is not feasible).
- Consider referral for coronary angiography if stress test is positive or if symptoms worsen.
- Continue current medications: Amlodipine 10mg daily and Simvastatin 20mg daily.
- Advised patient to avoid strenuous activity until further evaluation is complete.
Communication with Requesting Physician: Phone call made to Dr. Lee on 2025-06-18 at 10:15 AM to discuss initial assessment and recommendations.
Follow-Up Plan (if any): Patient to schedule cardiac stress test at Cardiology Associates. Will forward the results and further recommendations to Dr. Lee upon completion of testing.
Consulting Physician Signature: (Imagine a signature is drawn here)
Printed Name of Consulting Physician: Michael Brown
Specialty: Cardiology
Date: 2025-06-18
FAQs about the Consultation Note Template
Who typically initiates a consultation and completes the note?
The requesting physician initiates the consultation, but the consulting physician is responsible for documenting their findings, assessment, and recommendations in the consultation note.
What kind of information should be included in a consultation note?
Key elements include the requesting and consulting physician's information, patient details, the reason for consultation, relevant history, examination findings, review of records, the consultant's assessment and specific recommendations, communication details, and any follow-up plans.
How is a consultation note different from a referral note?
A referral note simply directs the patient to a specialist for evaluation or treatment. A consultation note documents the specific advice and recommendations provided by the specialist to the requesting physician regarding the patient's care.
Why are consultation notes important?
They ensure clear communication and collaboration between healthcare providers, provide expert guidance for managing complex cases, contribute to better patient outcomes, and serve as an important part of the patient's medical record.
Are there different ways a consultation can occur and be documented?
Yes, consultations can happen in person, via phone, or through electronic health record systems. The method of consultation might be noted in the communication section of the note.
Free Download: Printable Consultation Note Template
You can download the Consultation Note Template mentioned above by clicking Use Template button on this page. Customize it to fit your specific needs and preferences.