In the fast-paced world of healthcare, clear and concise documentation is paramount. One of the most widely used methods for structuring patient information is the SOAP note. This standardized format helps healthcare professionals organize their thoughts, communicate effectively, and ensure comprehensive record-keeping. If you're a healthcare student, a new practitioner, or simply interested in understanding medical documentation, this article will provide a detailed overview of the SOAP note template and its key components.
The SOAP note template is a structured approach to documenting patient encounters. It provides a systematic way for healthcare providers to record relevant information about a patient's condition, their assessment, and the plan of care. This format ensures that all critical aspects of a patient's visit are documented in a logical and easy-to-follow manner. The SOAP note promotes clarity and consistency in medical records, which is essential for effective communication among healthcare team members and for providing quality patient care.
What are SOAP notes?
SOAP notes are a method of documentation employed by healthcare providers to write out notes on a patient encounter. They are a fundamental part of the patient's medical record and serve as a communication tool between different healthcare professionals involved in the patient's care. The structured format helps to ensure that all relevant information is captured and organized logically.
What does SOAP stand for?
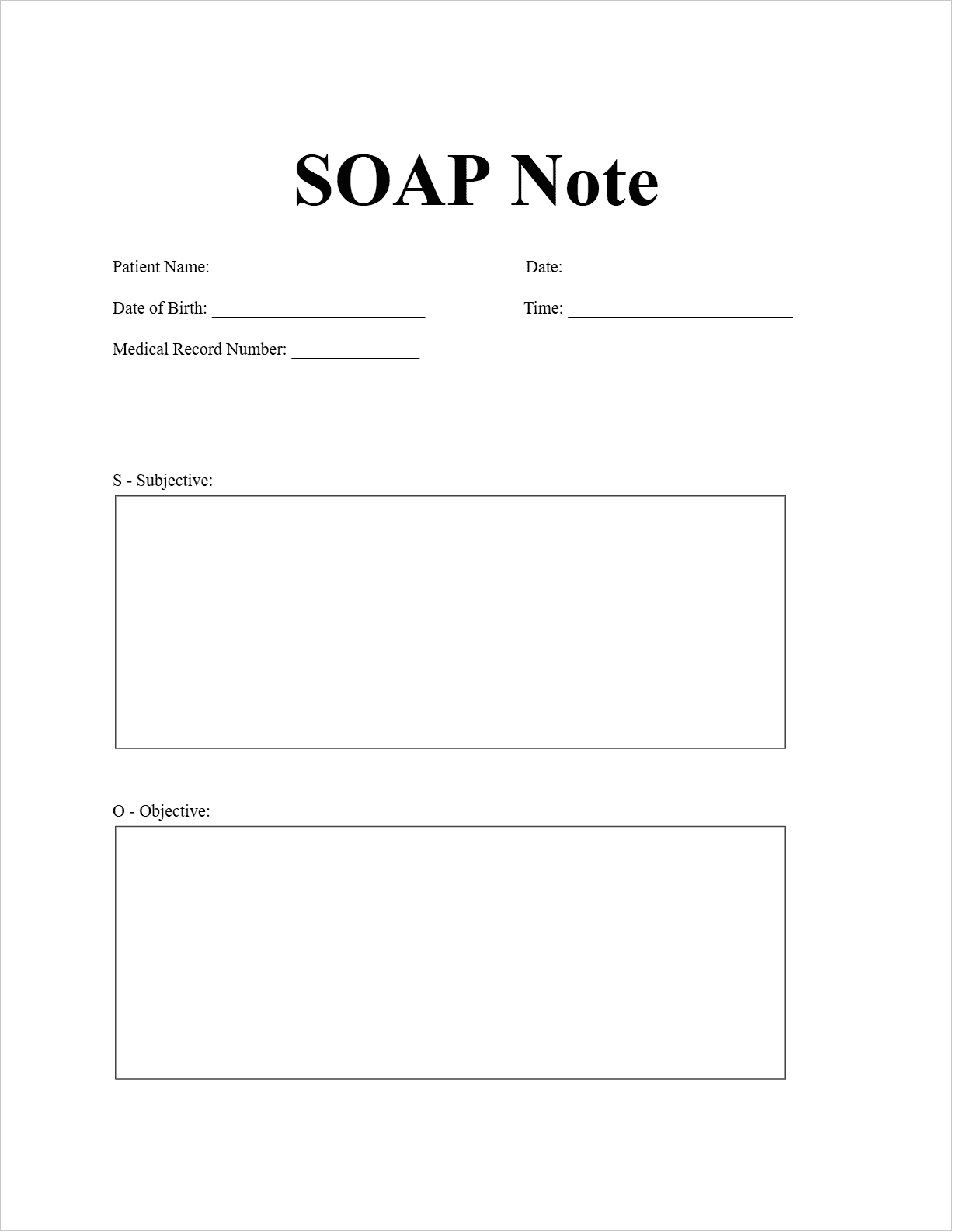
SOAP is an acronym that represents the four key components of the note:
- S - Subjective: This section includes information provided by the patient or their caregiver. It captures the patient's perspective, including their chief complaint, history of the present illness, past medical history, medications, allergies, social history, and family history.
- O - Objective: This section contains factual information obtained through the healthcare provider's observations, examinations, and diagnostic tests. It includes vital signs, physical examination findings, laboratory results, and imaging results.
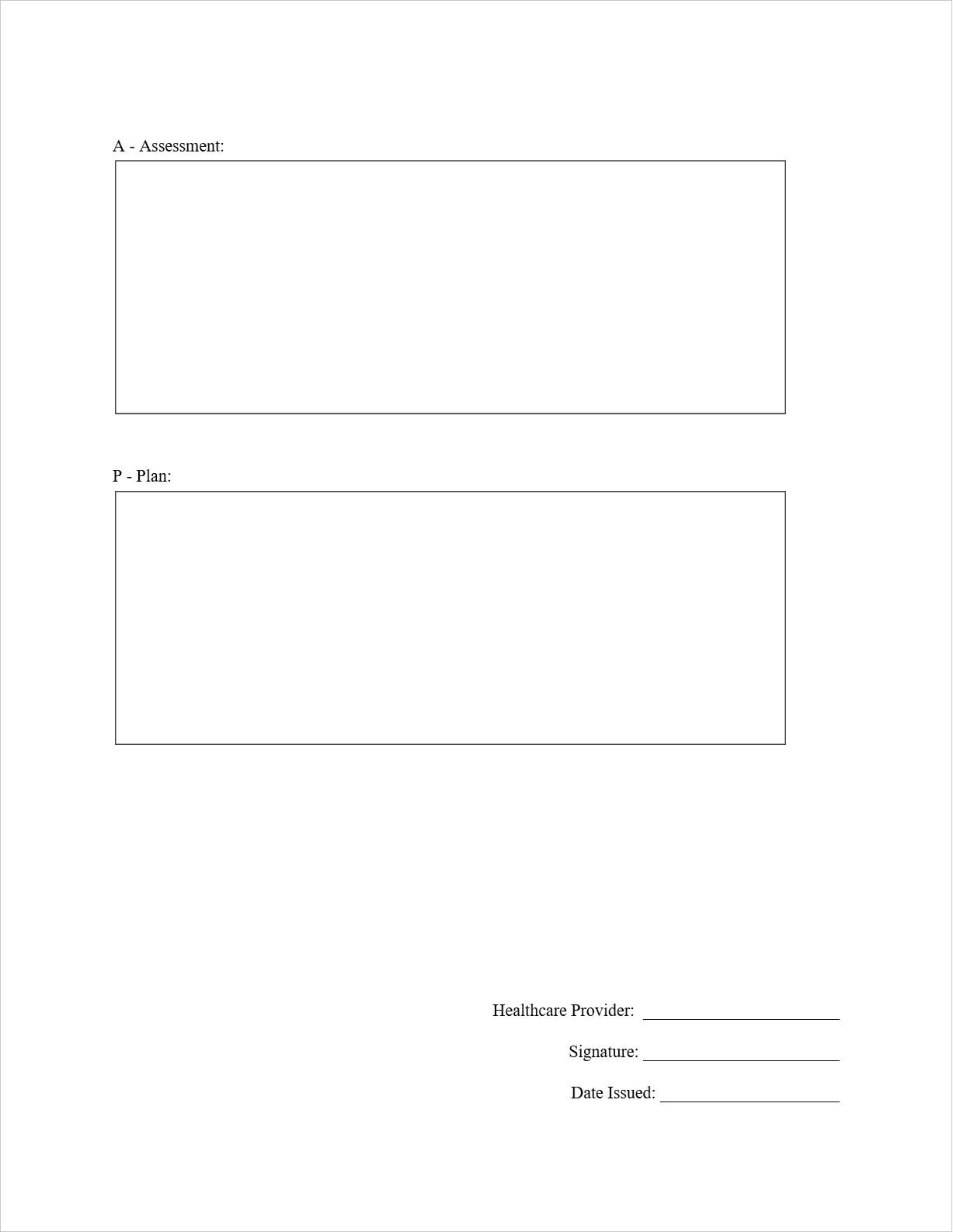
- A - Assessment: This section represents the healthcare provider's interpretation of the subjective and objective data. It includes the diagnosis or a list of possible diagnoses (differential diagnoses) based on the gathered information.
- P - Plan: This section outlines the course of action the healthcare provider will take to address the patient's condition. It includes the treatment plan, medications prescribed, therapies recommended, further testing ordered, and follow-up instructions.
SOAP Note Key Components
Let's break down each component of the SOAP note in more detail:
- Subjective (S): This is where you document what the patient tells you. It should include their main reason for the visit (chief complaint) in their own words. You'll also record the history of their current problem, details about past illnesses, current medications, any allergies, relevant social factors like lifestyle habits, and family medical history that might be pertinent to their current condition.
- Objective (O): This section focuses on what you observe and find during your examination and through diagnostic tests. It includes vital signs (blood pressure, heart rate, temperature, etc.), findings from your physical examination of different body systems, and the results of any lab work or imaging studies that have been performed.
- Assessment (A): This is your professional judgment of the patient's condition. Based on the subjective and objective information, you'll formulate a diagnosis or a list of potential diagnoses. You might also include a brief analysis of the patient's progress or any contributing factors to their condition.
- Plan (P): This section details what you intend to do for the patient. It includes the specific treatment plan, such as prescribing medications (including dosage and frequency), recommending therapies (like physical therapy or counseling), ordering further tests or procedures, and providing instructions for follow-up care. Patient education is also an important part of the plan.
When to use SOAP notes?
SOAP notes are a versatile and essential documentation method for a wide array of patient encounters in various healthcare settings. Here are some common situations where utilizing the SOAP note template is particularly beneficial:
- Routine Patient Visits: This is perhaps the most frequent scenario. Whether it's a check-up with a primary care physician, a follow-up with a specialist, or a regular appointment for chronic condition management, SOAP notes provide a structured way to record the patient's current status, any changes since the last visit, and the ongoing plan of care. This ensures continuity and helps track the patient's health over time.
- Initial Assessments: When a patient is seen for a new complaint or condition, a SOAP note is crucial for capturing the initial presentation. The subjective section will detail the onset and progression of symptoms, while the objective section records the baseline examination findings. The assessment will formulate the initial diagnosis or differential diagnoses, and the plan will outline the initial steps for investigation and management.
- Follow-Up Appointments: These visits are essential for monitoring the effectiveness of a treatment plan. A SOAP note helps to track the patient's response to interventions. The subjective section will include the patient's report on how they've been feeling and any changes in their symptoms. The objective section will document any relevant changes in vital signs or physical exam findings, and the plan will detail any necessary adjustments to the treatment.
- Consultations with Specialists: When a primary care physician refers a patient to a specialist, a SOAP note can be used by the specialist to document their findings and recommendations. This note provides valuable information back to the referring physician, ensuring coordinated care. The SOAP note will clearly outline the specialist's assessment and their proposed plan, which might include specific treatments or further investigations.
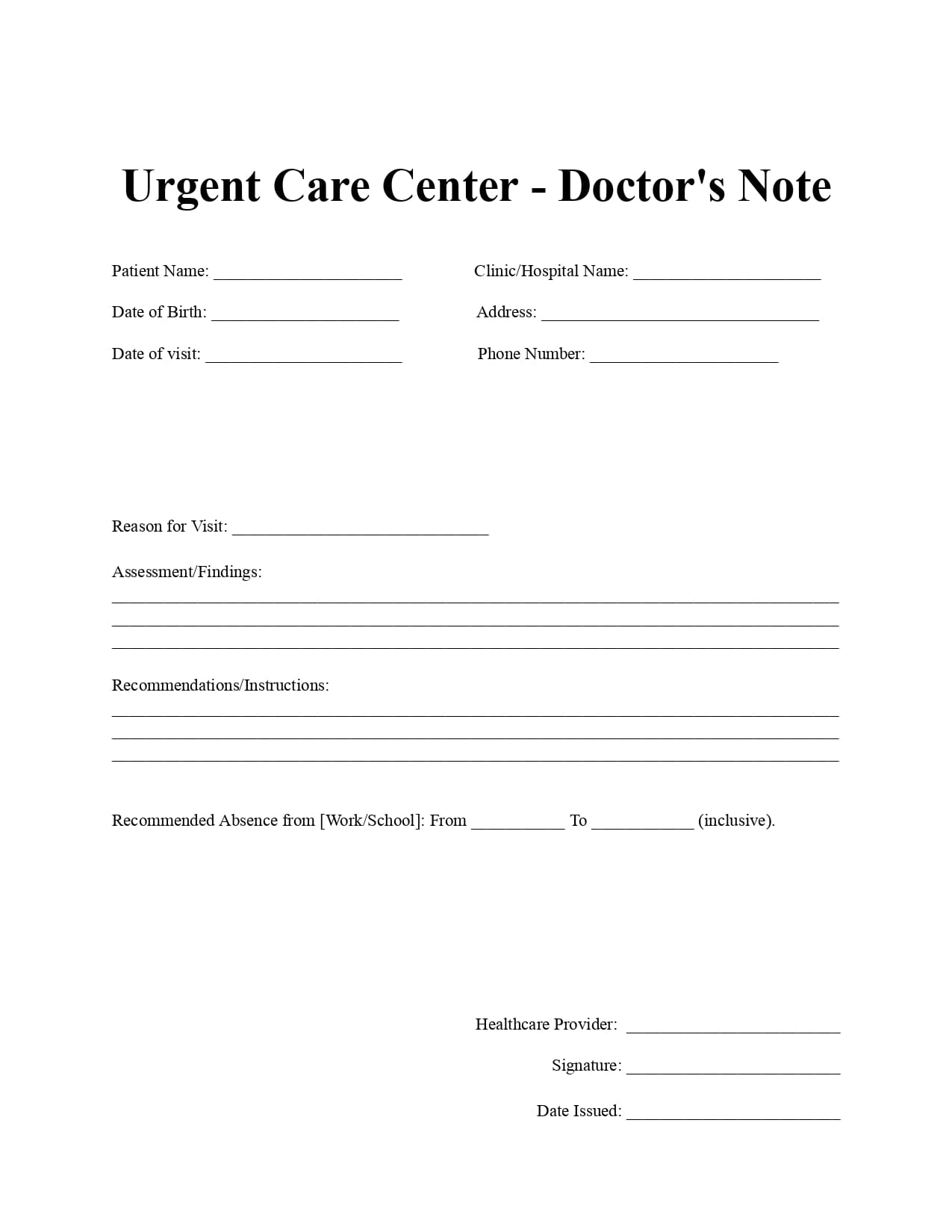
- Documenting Urgent Care or Emergency Encounters: Even in situations where time is critical, a concise SOAP note can efficiently capture the essential information from an urgent care visit or an initial evaluation in the emergency department. It allows for quick documentation of the presenting problem, key findings, the immediate assessment, and the initial management plan, which is crucial for subsequent healthcare providers.
In essence, SOAP notes are valuable whenever a healthcare professional interacts with a patient and needs to create a clear, organized, and comprehensive record of that encounter. Their structured format ensures that all vital information is captured, facilitating effective communication and informed decision-making for optimal patient care.
SOAP Note Example
Imagine a patient named John Davis visited Dr. Eleanor Ramirez for a follow-up appointment regarding his hypertension. Here's how their SOAP note might look:
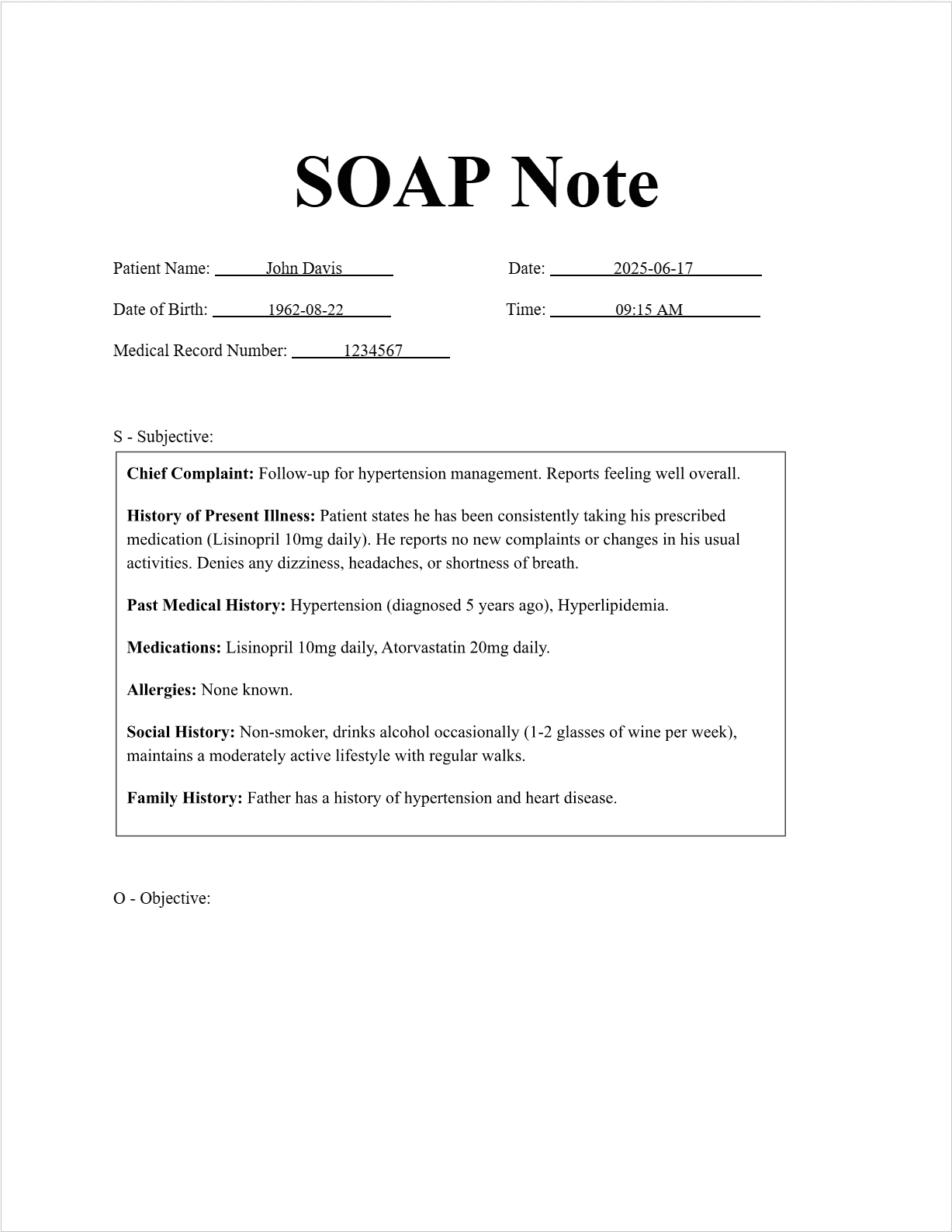
SOAP Note
Patient Information:
Patient Name: John Davis
Date of Birth: 1962-08-22
Medical Record Number: 1234567
Date and Time:
Date: 2025-06-17
Time: 09:15 AM
S - Subjective:
Chief Complaint: Follow-up for hypertension management. Reports feeling well overall.
History of Present Illness: Patient states he has been consistently taking his prescribed medication (Lisinopril 10mg daily). He reports no new complaints or changes in his usual activities. Denies any dizziness, headaches, or shortness of breath.
Past Medical History: Hypertension (diagnosed 5 years ago), Hyperlipidemia.
Medications: Lisinopril 10mg daily, Atorvastatin 20mg daily.
Allergies: None known.
Social History: Non-smoker, drinks alcohol occasionally (1-2 glasses of wine per week), maintains a moderately active lifestyle with regular walks.
Family History: Father has a history of hypertension and heart disease.
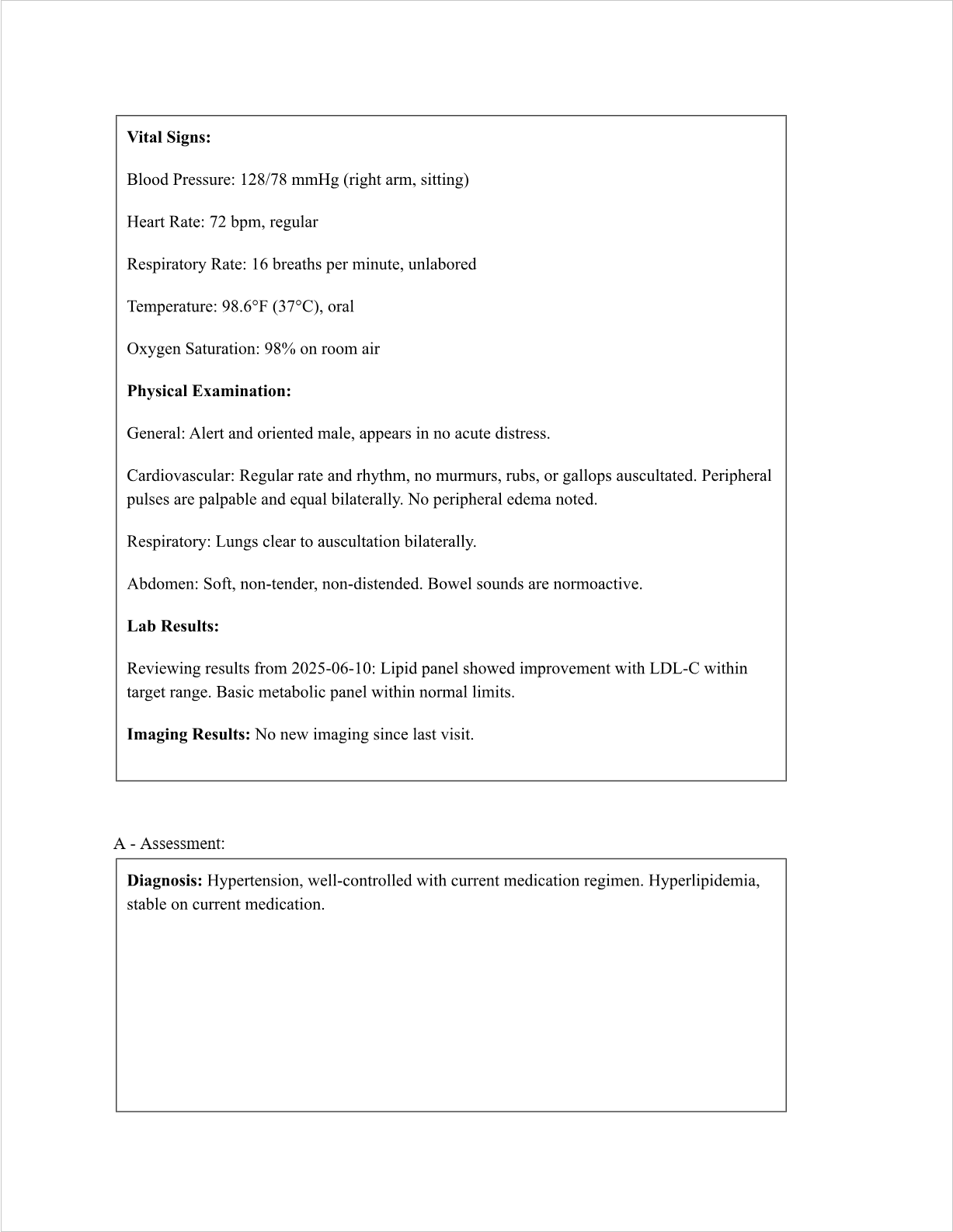
O - Objective:
Vital Signs:
Blood Pressure: 128/78 mmHg (right arm, sitting)
Heart Rate: 72 bpm, regular
Respiratory Rate: 16 breaths per minute, unlabored
Temperature: 98.6°F (37°C), oral
Oxygen Saturation: 98% on room air
Physical Examination:
General: Alert and oriented male, appears in no acute distress.
Cardiovascular: Regular rate and rhythm, no murmurs, rubs, or gallops auscultated. Peripheral pulses are palpable and equal bilaterally. No peripheral edema noted.
Respiratory: Lungs clear to auscultation bilaterally.
Abdomen: Soft, non-tender, non-distended. Bowel sounds are normoactive.
Lab Results:
Reviewing results from 2025-06-10: Lipid panel showed improvement with LDL-C within target range. Basic metabolic panel within normal limits.
Imaging Results:
No new imaging since last visit.
A - Assessment:
Diagnosis: Hypertension, well-controlled with current medication regimen. Hyperlipidemia, stable on current medication.
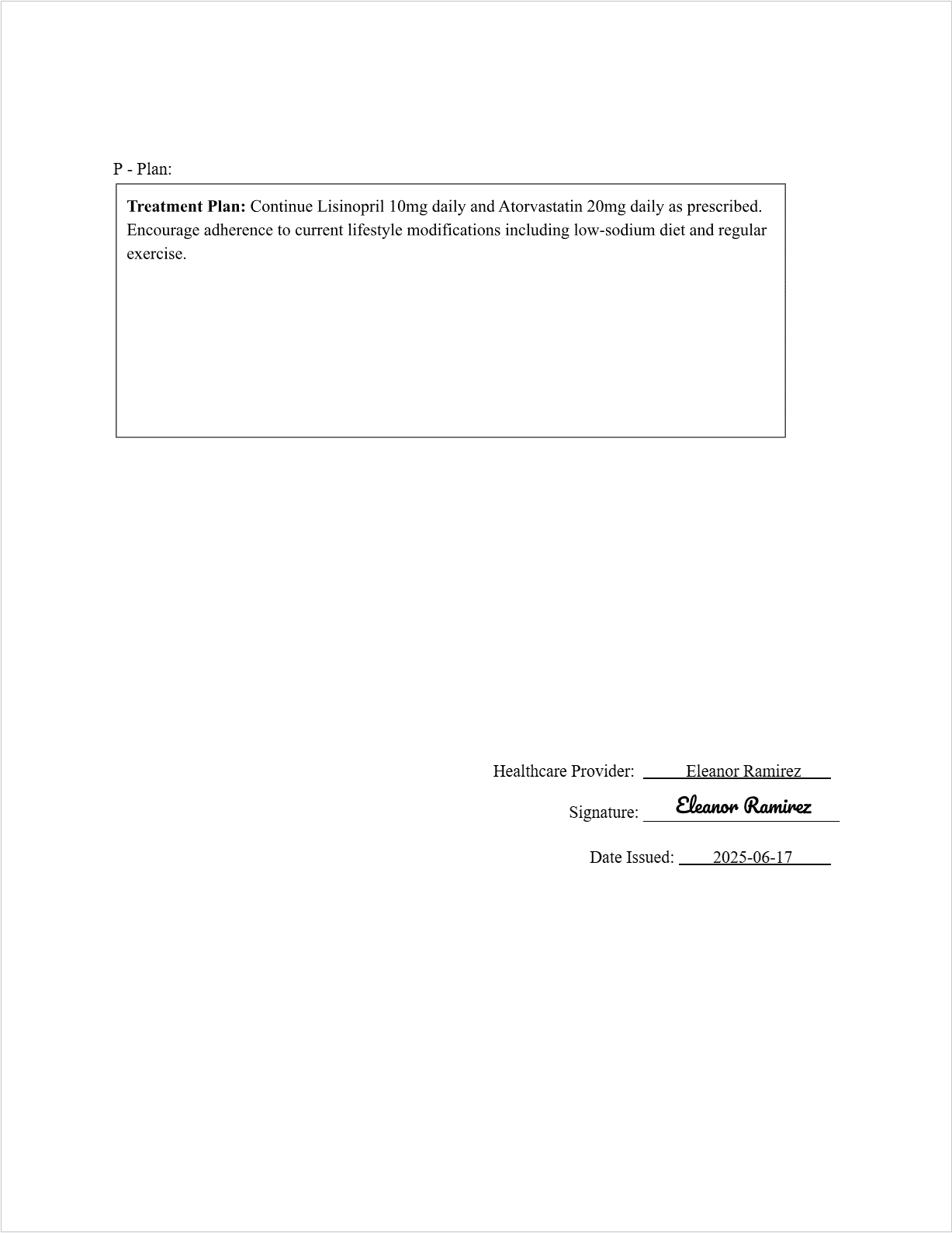
P - Plan:
Treatment Plan: Continue Lisinopril 10mg daily and Atorvastatin 20mg daily as prescribed. Encourage adherence to current lifestyle modifications including low-sodium diet and regular exercise.
Follow-Up: Schedule follow-up appointment in 3 months for routine monitoring of blood pressure and lipid levels. Patient instructed to contact the office sooner if any new symptoms develop.
Healthcare Provider Information:
Healthcare Provider Name: Eleanor Ramirez
Signature: (Imagine a signature is drawn here)
Date: 2025-06-17
FAQs about the SOAP Note Template
Is there a specific format I must follow for a SOAP note?
While the basic SOAP structure is standard, individual clinics or institutions may have their own specific templates or variations they prefer. It's best to adhere to the guidelines of your specific workplace or educational program.
How detailed should each section of the SOAP note be?
The level of detail will depend on the complexity of the patient's condition and the purpose of the note. It should be comprehensive enough to provide a clear picture of the patient's encounter and the plan of care.
Can SOAP notes be electronic?
Absolutely! Many electronic health record (EHR) systems incorporate SOAP note templates, making documentation more efficient and accessible.
Are SOAP notes only for doctors?
No, SOAP notes can be used by various healthcare professionals, including nurses, therapists, and counselors, adapting the content to their specific roles and patient interactions.
What are the benefits of using the SOAP note template?
The SOAP note template promotes organization, improves communication among healthcare providers, ensures comprehensive documentation, facilitates critical thinking, and helps in tracking patient progress over time.
By understanding and utilizing the SOAP note template, healthcare professionals can enhance the quality and efficiency of their patient documentation, ultimately leading to improved patient care.
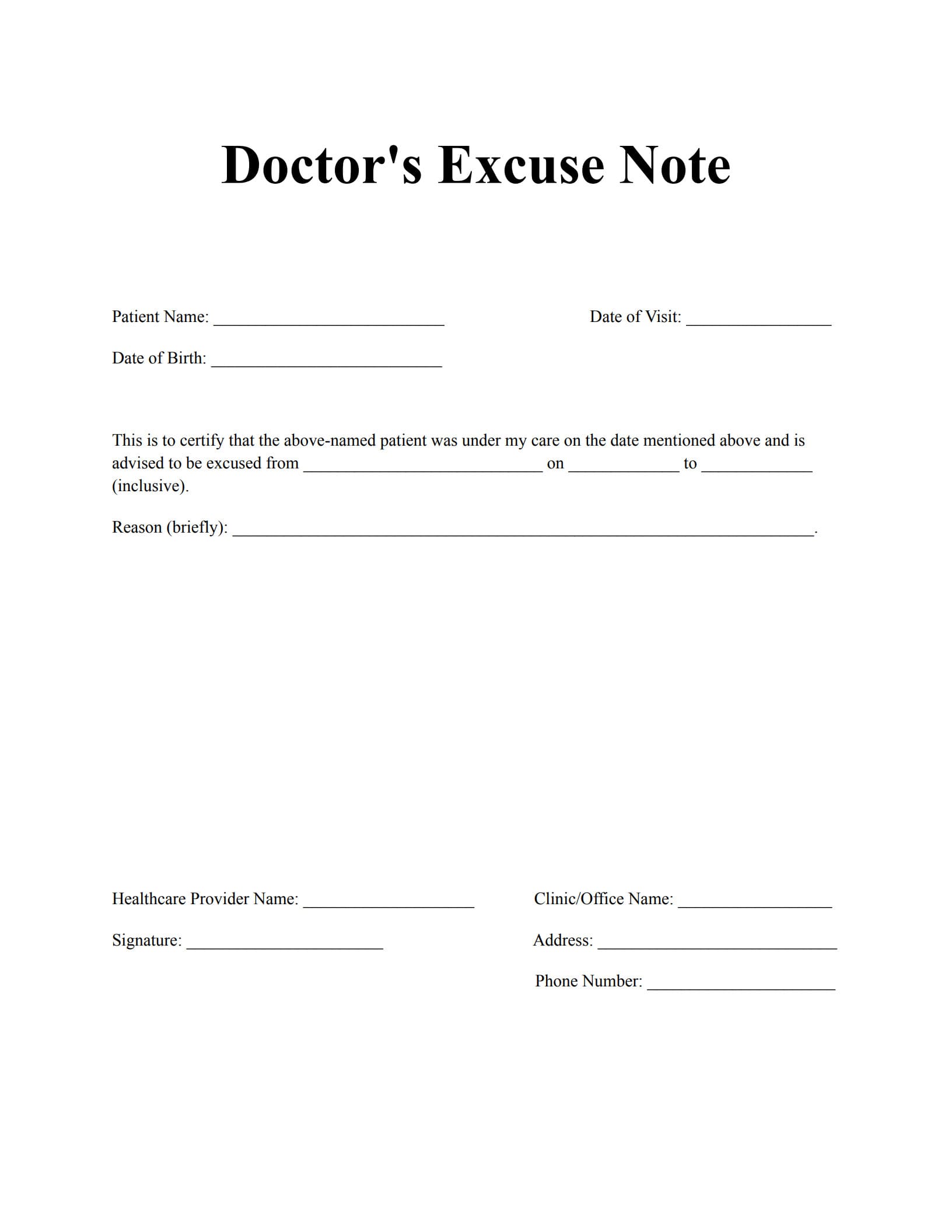
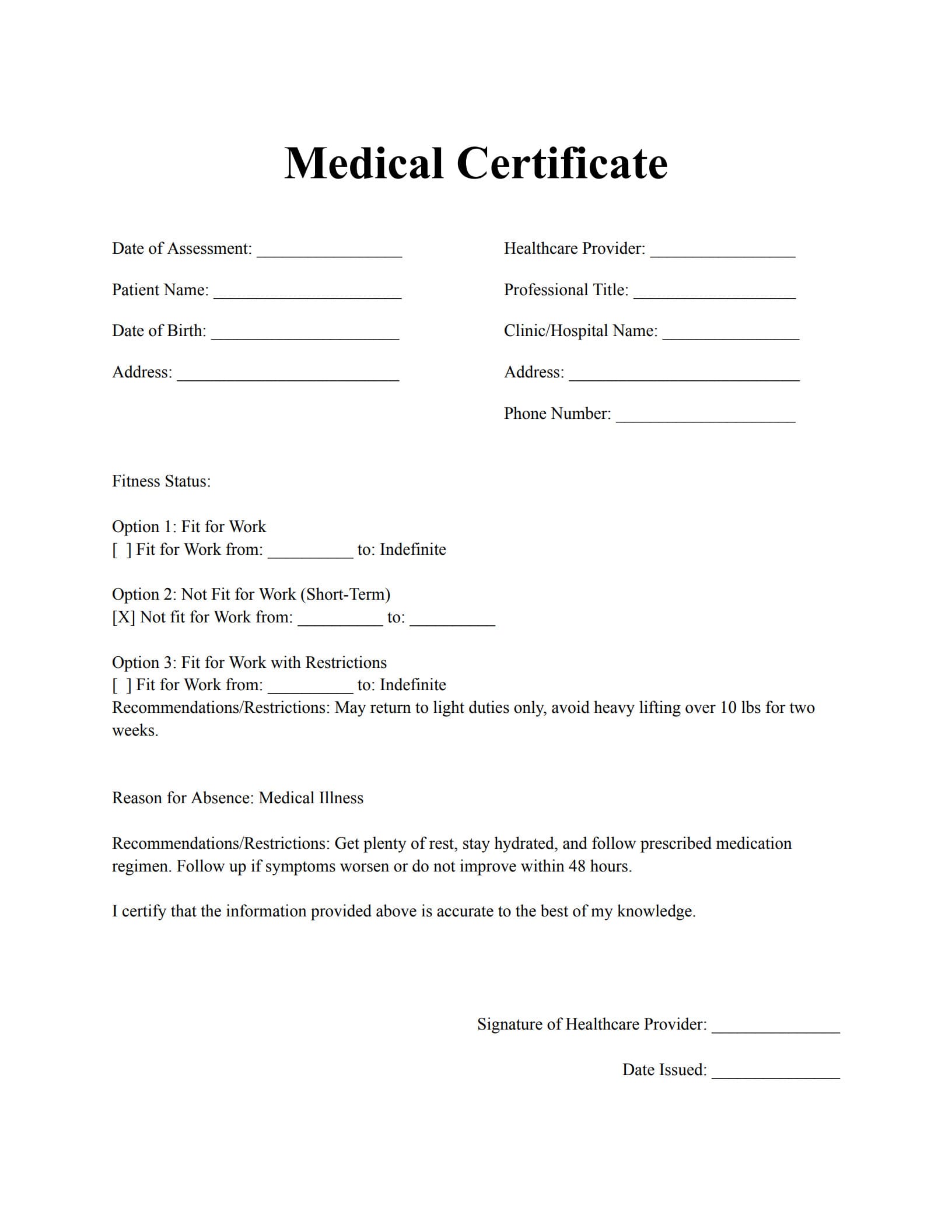
Free Download: Printable SOAP Note Template
You can download the SOAP Note template mentioned above by clicking Use Template button on this page. Customize them to fit your specific needs and preferences.