The moment a patient is ready to leave the hospital marks a significant milestone in their care journey. However, a crucial step in ensuring their continued recovery and well-being is the creation of a comprehensive discharge summary. This document serves as a roadmap for the patient and their primary care physician, outlining the key events of their hospital stay and the necessary steps for post-discharge care. This article will explore the essential components of a Discharge Summary template and highlight its importance in facilitating a seamless transition back to daily life.
What is a Discharge Summary?
A Discharge Summary is a comprehensive report prepared by the discharging physician or healthcare team at the end of a patient's hospital stay. It provides a concise yet thorough overview of the patient's admission, the treatment they received, their condition upon discharge, and detailed instructions for follow-up care. This document acts as a vital communication tool, ensuring that the patient and their primary care physician have all the necessary information to manage their health effectively after leaving the hospital.
What are the differences between a Discharge Summary and an After Visit Summary?
While both documents provide information to patients after a medical encounter, they serve different purposes and contain varying levels of detail:
- Discharge Summary: This document is prepared at the end of a hospital stay (which can range from a few days to weeks or even months). It offers a comprehensive overview of the entire hospitalization, including the admitting diagnosis, hospital course, procedures performed, discharge diagnosis, medications, discharge instructions, and follow-up plans. It is a more extensive document.
- After Visit Summary (AVS): This is typically provided after an outpatient visit, such as a doctor's appointment or a visit to an urgent care center. It is a shorter document that summarizes the key points discussed during the visit, the assessment, and the immediate plan of care, including any new medications or follow-up instructions.
In essence, a Discharge Summary covers a more significant period of care and provides a broader overview than an After Visit Summary, which focuses on a single outpatient encounter.
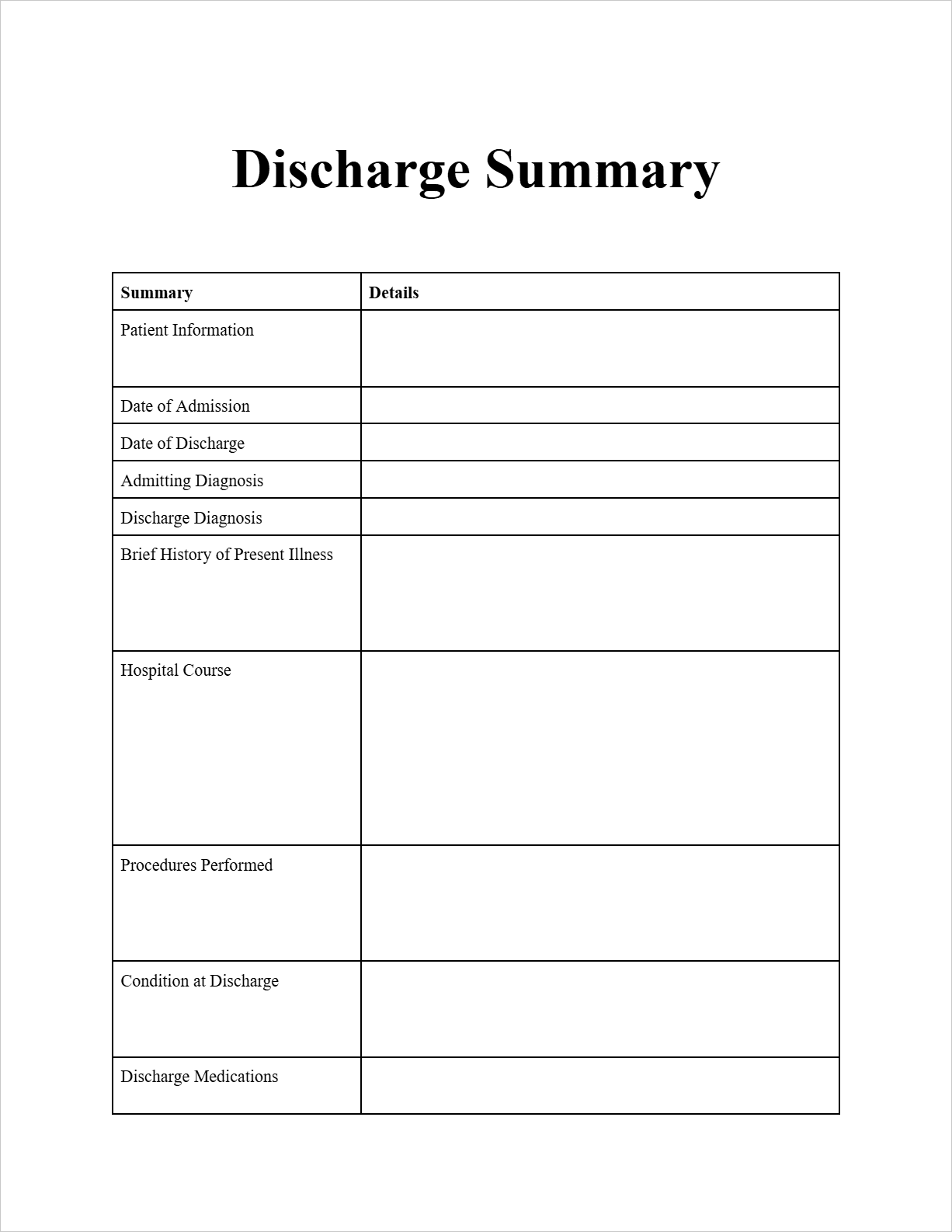
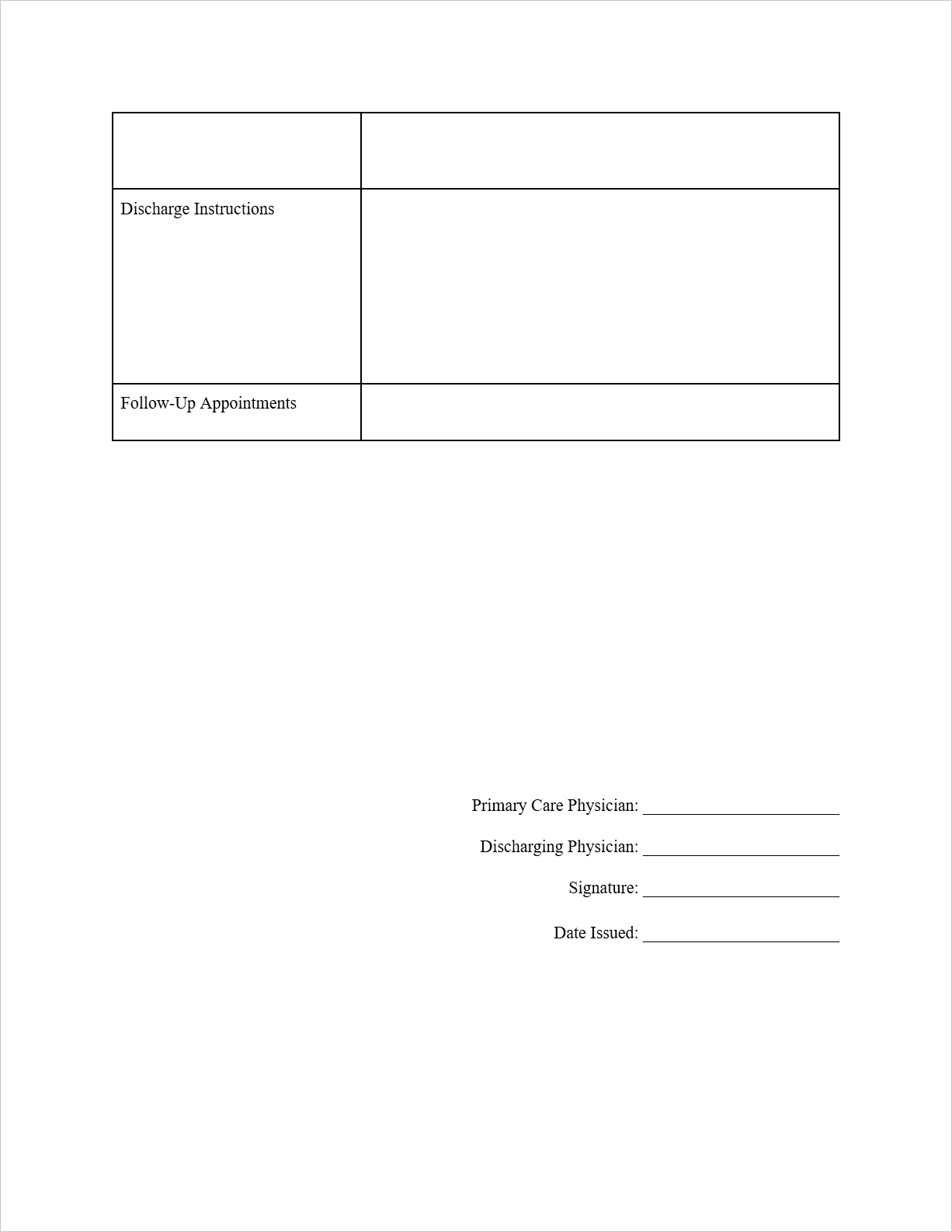
Key Components of a Discharge Summary Template
A well-structured Discharge Summary template typically includes the following essential sections:
- Patient Identification: Full name, date of birth, and medical record number.
- Admission and Discharge Information: Dates of admission and discharge.
- Admitting Diagnosis: The primary reason for the patient's hospitalization.
- Discharge Diagnosis: The final diagnosis determined at the time of discharge.
- Brief History of Present Illness: A concise summary of the medical issue that led to the patient's admission.
- Hospital Course: A narrative summary of the significant events, treatments, and the patient's progress throughout their hospital stay.
- Procedures Performed: A list of any surgical or significant medical procedures conducted during the hospitalization.
- Condition at Discharge: A brief statement describing the patient's overall health status at the time of release from the hospital (e.g., stable, improved).
- Discharge Medications: A complete list of all medications the patient needs to take after discharge, including dosages, frequency, and route of administration.
- Discharge Instructions: Detailed instructions for the patient to follow at home, which may include dietary recommendations, activity restrictions, wound care guidelines, and potential warning signs to watch out for.
- Follow-Up Care: Information regarding any necessary follow-up appointments with specialists or the primary care physician, including dates, times, and contact information.
- Primary Care Physician Information: The name of the patient's regular doctor.
- Information of the Discharging Physician: Name, signature, and date of the healthcare provider completing the summary.
Discharge Summary Example
Let's revisit our patient, Alice Johnson, who was hospitalized for pneumonia and is now being discharged:
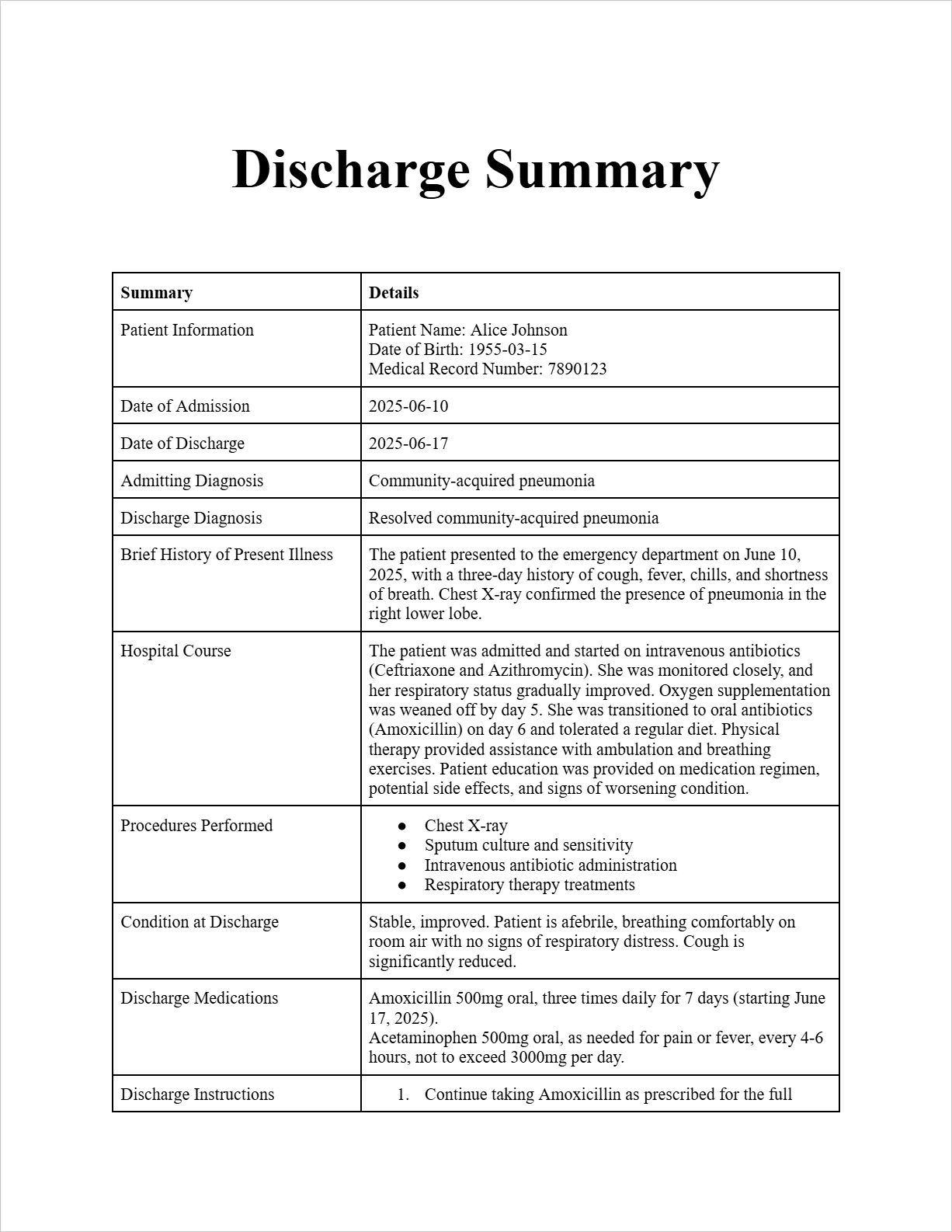
Discharge Summary
Patient Information:
Patient Name: Alice Johnson
Date of Birth: 1955-03-15
Medical Record Number: 7890123
Admission and Discharge Dates:
Date of Admission: 2025-06-10
Date of Discharge: 2025-06-17
Admitting Diagnosis: Community-acquired pneumonia
Discharge Diagnosis: Resolved community-acquired pneumonia
Brief History of Present Illness: The patient presented to the emergency department on June 10, 2025, with a three-day history of cough, fever, chills, and shortness of breath. Chest X-ray confirmed the presence of pneumonia in the right lower lobe.
Hospital Course: The patient was admitted and started on intravenous antibiotics (Ceftriaxone and Azithromycin). She was monitored closely, and her respiratory status gradually improved. Oxygen supplementation was weaned off by day 5. She was transitioned to oral antibiotics (Amoxicillin) on day 6 and tolerated a regular diet. Physical therapy provided assistance with ambulation and breathing exercises. Patient education was provided on medication regimen, potential side effects, and signs of worsening condition.
Procedures Performed:
- Chest X-ray
- Sputum culture and sensitivity
- Intravenous antibiotic administration
- Respiratory therapy treatments
Condition at Discharge: Stable, improved. Patient is afebrile, breathing comfortably on room air with no signs of respiratory distress. Cough is significantly reduced.
Discharge Medications:
- Amoxicillin 500mg oral, three times daily for 7 days (starting June 17, 2025).
- Acetaminophen 500mg oral, as needed for pain or fever, every 4-6 hours, not to exceed 3000mg per day.
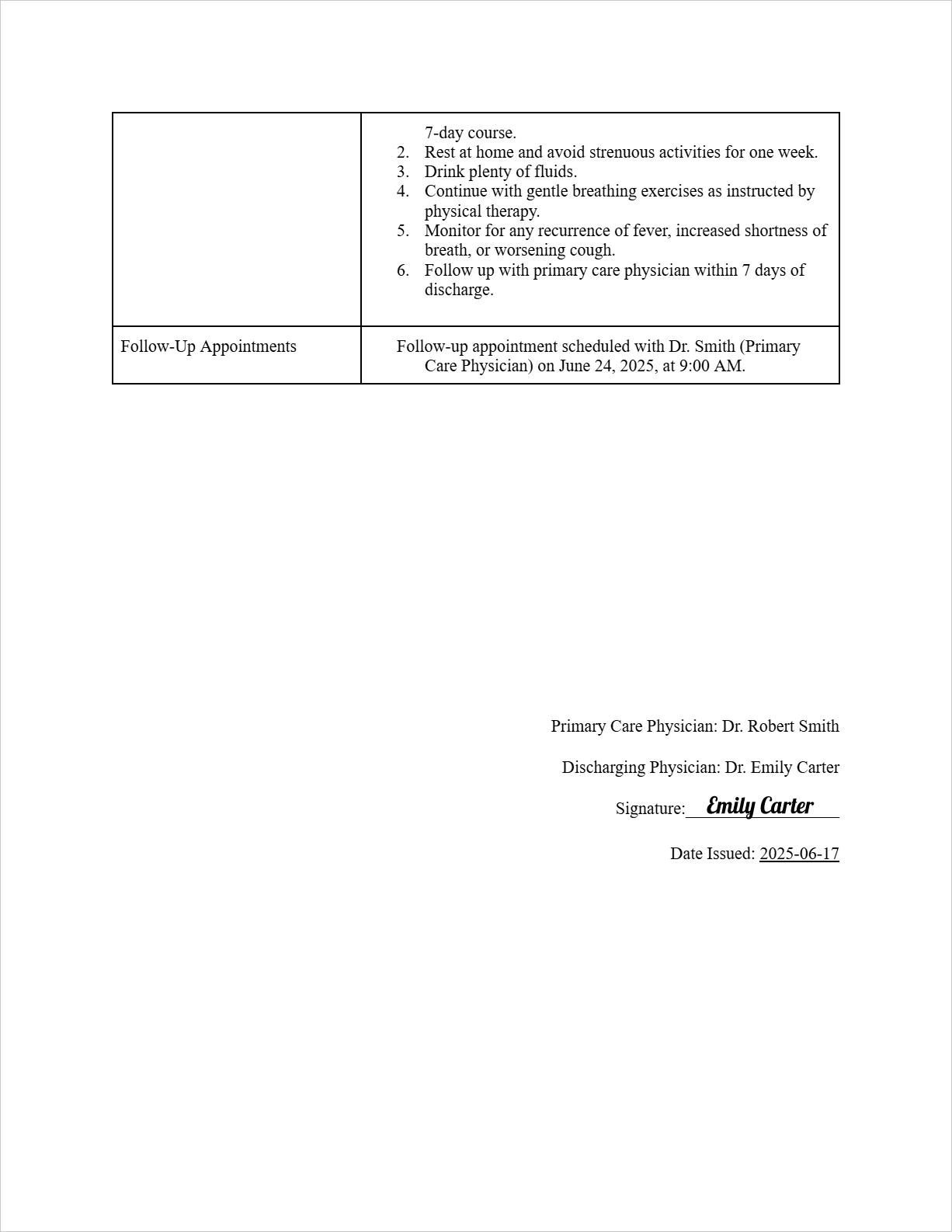
Discharge Instructions:
- Continue taking Amoxicillin as prescribed for the full 7-day course.
- Rest at home and avoid strenuous activities for one week.
- Drink plenty of fluids.
- Continue with gentle breathing exercises as instructed by physical therapy.
- Monitor for any recurrence of fever, increased shortness of breath, or worsening cough.
- Follow up with primary care physician within 7 days of discharge.
Follow-Up Appointments:
Follow-up appointment scheduled with Dr. Smith (Primary Care Physician) on June 24, 2025, at 9:00 AM.
Primary Care Physician:
Name: Dr. Robert Smith
Healthcare Provider Information (Discharging Physician):
Discharging Physician Name: Dr. Emily Carter
Signature: (Imagine a signature is drawn here)
Date: 2025-06-17
FAQs about the Discharge Summary Template
Who is responsible for preparing the Discharge Summary?
Typically, the discharging physician or another designated member of the patient's healthcare team prepares the discharge summary.
When should the Discharge Summary be completed?
Ideally, the discharge summary should be completed within 24-48 hours of the patient's discharge to ensure timely communication with the primary care physician.
How is the Discharge Summary shared?
The discharge summary is usually provided to the patient upon discharge and a copy is also sent to their primary care physician. Electronic health records have made this process more efficient.
Why is a Discharge Summary so important?
It ensures continuity of care, provides essential information for managing the patient's health at home, reduces the risk of readmission, and serves as a legal document of the patient's hospital stay.
Can patients access their Discharge Summary?
Yes, patients have a right to access their medical records, including the discharge summary. Healthcare facilities have policies and procedures for patients to request copies of their records.
Free Download: Printable Discharge Summary Template
You can download the Discharge Summary template mentioned above by clicking Use Template button on this page. Customize it to fit your specific needs and preferences.